Hand Hygiene
OVERVIEW
- Hand hygiene is endorsed by the WHO as the single most important element of strategies to preventing healthcare associated infection (HAI)
- It is the responsibility of every healthcare worker (HCW)
- The recommendations on this page are based on those of Hand Hygiene Australia
REQUIREMENTS FOR TRANSMISSION OF INFECTIOUS AGENTS BY HAND
- Organisms are present on the patient’s skin, or have been shed onto inanimate objects immediately surrounding the patient
- Organisms must be transferred to the hands of the HCWs
- Organisms must be capable of surviving for at least several minutes on HCWs’ hands
- Hand washing or hand rubbing by the HCW must be inadequate or entirely omitted, or the agent used for hand hygiene inappropriate
- The contaminated hand or hands of the caregiver must come into direct contact with another patient or with an inanimate object that will come into direct contact with the patient
TARGETS
Hand hygiene targets prevention of the following:
- cross-colonisation of patients
- endogenous and exogenous infection in patients
- infection in HCWs
- cross-colonisation of the healthcare environment including HCWs
WHEN
The timing of hand hygiene episodes is more important than their frequency.
Hand hygiene must be performed before and after every episode of patient contact. This includes the ‘5 moments of hand hygiene’:
- before touching a patient
- before a procedure
- after a procedure or body substance exposure risk
- after touching a patient
- after touching a patient’s surroundings
Hand Hygiene must be performed:
- on entering the patient zone from the healthcare zone (this includes after closing the screens as they are potentially contaminated)
- between touching the patient and touching the critical sites on the same patient (e.g. IV site and drain sites)
- before leaving the patient zone
-> Any equipment brought into the patient zone should be cleaned before and after each patient use eg. stethoscope, BP cuff, tourniquet etc.
Hand hygiene must also be performed:
- after removal of gloves
- before/ after work
- before/ after eating/ drinking
- before/ after using a keyboard
- after visiting an infected area
- after toileting
- after wiping/ blowing nose
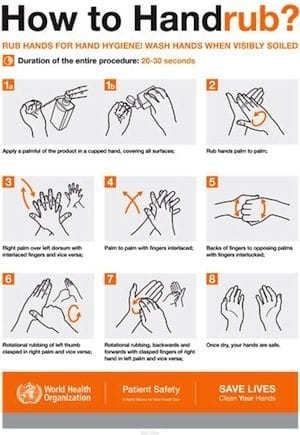
HOW
For all routine hand hygiene practices in healthcare settings, use alcohol-based hand rubs that :
- contain between 60% and 80% v/v ethanol or equivalent
- meet the requirements of the EN1500 standard (a different standard is used in North America)
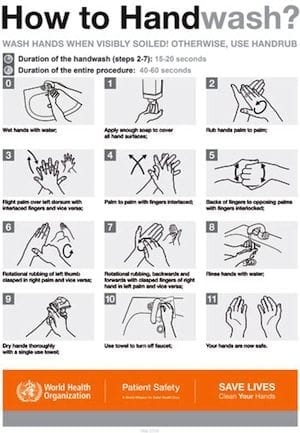
If hands are visibly soiled:
- use soap and water
If known or suspected Clostridium difficile and non-enveloped viruses (e.g. norovirus):
- use soap and water if gloves have not been worn
- After washing, hands should be dried thoroughly with single-use towels
GLOVES
Gloves are indicated to:
- Reduce the risk of contamination of HCWs hands with blood and other body fluids
- Prevent the transmission of infectious microorganisms via the healthcare workers hands to the environment, to the patient, as well as from one patient to another
Wearing gloves does not replace the need for hand hygiene
- perform hand hygiene before and after glove use
Change gloves:
- Between episodes of care for different patients, to prevent transmission of infectious material
- During the care of a single patient, to prevent cross-contamination of body sites
- If the patient interaction involves touching portable computer keyboards or other mobile equipment that is transported from room to room
- Sterile gloves must be used for surgical ANTT (‘aseptic, no touch technique’) procedures and contact with sterile sites
BARRIERS TO HAND HYGIENE
HCWs must not wear artificial nails or extenders when having direct contact with patients and natural nails should be kept short (<0.4cm long)
- Artificial, painted and chipped nails can harbour microbes and are linked to outbreaks
Avoid the wearing of hand and wrist jewellery
- they can be heavily colonised and are usually not removed for hand hygiene
Skin care
- Provide HCWs with hand lotions or creams to minimise the occurrence of irritant contact dermatitis associated with hand antisepsis or hand washing
- Provide alternative hand hygiene products for HCWs with confirmed allergies or adverse reactions to standard products used in the healthcare setting
VIDEO
NEJM video on hand hygiene:
HHA’s ‘5 moments of hand hygiene’ video:
References and Links
LITFL
- CCC — Standard precautions
- CCC — Transmission-based precautions
- CCC — Handwashing in the ICU
- Why don’t we wash our hands? (presentation by Chris Nickson at SMACC Chicago, 2015)
Textbooks and journal articles
- Azim S, McLaws ML. Doctor, do you have a moment? National Hand Hygiene Initiative compliance in Australian hospitals. Med J Aust. 2014;200:(9)534-7. [pubmed]
- Gilbert GL. One moment doctor! Have you forgotten hand hygiene? Med J Aust. 2014;200:(9)508-9. [pubmed]
- Grayson ML, Melvani S, Druce J, et al. Efficacy of soap and water and alcohol-based hand-rub preparations against live H1N1 influenza virus on the hands of human volunteers. Clin Infect Dis. 2009;48:(3)285-91. [pubmed]
- Jabbar U, Leischner J, Kasper D, et al. Effectiveness of alcohol-based hand rubs for removal of Clostridium difficile spores from hands. Infect Control Hosp Epidemiol. 2010;31:(6)565-70. [pubmed]
- Larson E. Monitoring hand hygiene: meaningless, harmful, or helpful? Am J Infect Control. 2013;41:(5 Suppl)S42-5. [pubmed]
- Pittet D, Allegranzi B, Sax H, Dharan S, Pessoa-Silva CL, Donaldson L, Boyce JM; WHO Global Patient Safety Challenge, World Alliance for Patient Safety. Evidence-based model for hand transmission during patient care and the role of improved practices. Lancet Infect Dis. 2006 Oct;6(10):641-52. [pubmed]
- Pittet D, Dharan S, Touveneau S, Sauvan V, Perneger TV. Bacterial contamination of the hands of hospital staff during routine patient care. Arch Intern Med. 1999;159:(8)821-6. [pubmed]
- Pittet D, Hugonnet S, Harbarth S, et al. Effectiveness of a hospital-wide programme to improve compliance with hand hygiene. Infection Control Programme. Lancet. 2000;356:(9238)1307-12. [pubmed]
- Sax H, Allegranzi B, Uçkay I, Larson E, Boyce J, Pittet D. ‘My five moments for hand hygiene’: a user-centred design approach to understand, train, monitor and report hand hygiene. J Hosp Infect. 2007 Sep;67(1):9-21.[pubmed]
- Tschudin-Sutter S, Pargger H, Widmer AF. Hand hygiene in the intensive care unit. Crit Care Med. 2010;38:(8 Suppl)S299-305. [pubmed]
FOAM and web resources
- Hand Hygiene Australia
- World Health Organisation. WHO Guidelines on Hand Hygiene in Health Care. In: World Alliance for Patient Safety, editor. First Global Patient Safety Challenge Clean Care is Safer Care. 1 ed. Geneva: World Health Organisation Press; 2009. [Website with access to free full text]
- Wi 5? game from the UK’s NHS (NB. there are slight regional differences in the 5 moments of hand hygiene; this is based on UK guidelines where aural and oral care is considered moment 2, rather than moment 1 as is the case in Australia)

Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC