Inotropes, vasopressors and other vasoactive agents
Reviewed and revised 9 September 2016
OVERVIEW
Vasoactive agents include the following:
- inotropes are agents that increase myocardial contractility (inotropy)
— e.g. adrenaline, dobutamine, isoprenaline, ephedrine - vasopressors are agents that cause vasoconstriction leading to increased systemic and/or pulmonary vascular resistance (SVR, PVR)
— e.g. noradrenaline, vasopressin, metaraminol, vasopressin, methylene blue - inodilators are agents with inotropic effects that also cause vasodilation leading to decreased systemic and/or pulmonary vascular resistance (SVR, PVR)
— e.g. milrinone, levosimendan - some agents don’t fit these categories easily!
— e.g. dopamine
No inotropic agents have been shown to have superiority over any others in good quality trials.
- Use is based on cost, availability, interpretation of physiology and personal/ institutional preference.
- More detail on each agent can be found by searching the Critical Care Compendium.
| Agent | Adrenaline | Noradrenaline | Dopamine | Dobutamine |
|---|---|---|---|---|
| Class | endogenous catecholamine | endogenous catecholamine | endogenous catecholamine | synthetic catecholamine |
| Mechanism | beta > alpha | alpha > beta | DA > beta > alpha | beta 1 and 2 |
| Effects | b1 -> +HR, +inotropy, +CO alpha at higher doses preserves coronary and cerebral blood flow b2 -> +vasodilation, +brochodilation | a1-> +SVR +beta at higher doses | dose (mcg/kg/h) 1-5 = DAR 1+2 5-10 = betaR >10 = alphaR + aldosterone | inotropy + VO2 + myocardial work mild + HR + coronary perfusion mild - SVR mild - PVR |
| Pharmacokinetics | onset in mins Met: COMT + MAO t/12 = mins | onset in mins Met: COMT + MAO t/12 = mins | onset in mins Met: COMT + MAO t/12 = mins | onset in mins methylation + conjugation t/12 = mins urine + bile -> inactive metabolites |
| Use | cardiac arrest low CO state cardiac surgery | septic shock vasodilation | nil (kids!) | low CO state part of EGDT cardiac surgery |
| Pros | $ titratable familiar available | $ titratable familiar available | $ titratable familiar available | titratable familiar available |
| Cons | lactic acidosis low K, low PO4 | reflex bradycardia hypertension peripheral ischemia | arrhythmia pulmonary vasoconstriction N&V immune dysregulation - TSH and PRL release | $$ myocardial ischemia tachydysrhythmias tachyphylaxis |
| Evidence | Annane 2007: vs dobtumine + norad = no difference in septic shock CAT: vs norad in septic shock = no difference | CAT: vs adrenaline in septic shock = no difference Annane 2007: with dobutamine vs adrenaline = no difference in septic shock | Bellomo 2000: no 'renal dose' dopamine De Backer 2010 and Patel 2010: vs norad = more tachydysrhythmias in septic shock | SURVIVE: no mortality benefit vs levosimendan Annane 2007: with norad vs adrenaline = no difference in septic shock |
| Agent | Vasopressin | Levosimendan | Milrinone |
|---|---|---|---|
| Class | endogenous peptide | calcium sensitiser (inodilator) | bipyridine inodilator |
| Mechanism | V1R = vasoconstriction V2R = renal + endothelium V3R = pituitary OTR = oxytoxin type receptors | modulates troponin C activates vascular ATP-dependent K channels | cAMP PDE-3 inhibitor |
| Effects | antidiuresis + SVR + platelet aggregation + PVR - splanchnic flow | inotropy - SVR - PVR +CO | |
| Pharmacokinetics | peptidases t1/2 = 10-20 min | slow onset (can give loading dose) liver + renal metabolism t1/2 = 1 hour but has active metabolites effects last up to 1/52 | t1/2 = 2.3h renal no effect >8h |
| Use | septic shock (cardiac arrest} | low CO state | low CO state cardiac surgery support RV |
| Pros | fast onset/ offset (except renal effects) catecholamine resistance | OK if b-blockers catacholamine resistance faster decrease in BNP cf. dobutamine | pulmonary vasodilation OK if b-blockers catacholamine resistance little +HR |
| Cons | $$$$ pulmonary hypertension splanchnic ischaemia uterine contraction ? thrombosis | $$$$$ tachycardia low BP headache not if LVOTO not if liver/ renal disease | $$$ hypotension may need norad little evidence |
| Evidence | VASST: no benefit vs norad in septic shock | SURVIVE: no mortality beneift vs dobutamine | faster weaning off bypass |
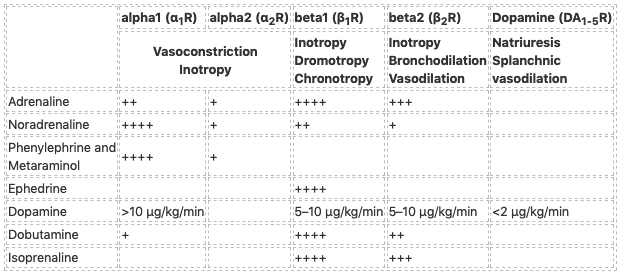
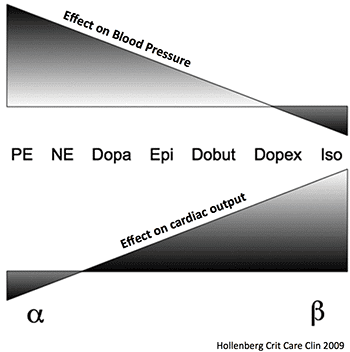
ACTIONS OF CATECHOLAMINES
From Senz and Nunnink:
These ‘textbook’ descriptions do not necessarily translate into clinical practice and effects may vary with dose and clinical status.
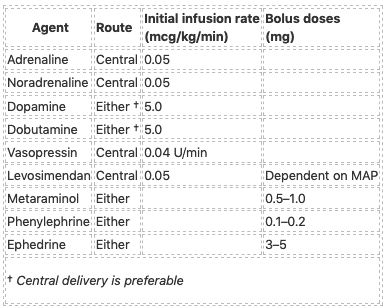
GUIDE TO INFUSIONS
From Senz and Nunnink:
References and Links
LITFL
- Search the CCC for individual agents.
Journal articles
- Bangash MN, Kong ML, Pearse RM. Use of inotropes and vasopressor agents in critically ill patients. Br J Pharmacol. 2012 Apr;165(7):2015-33. PMC3413841.
- Evans N. Which inotrope for which baby? Arch Dis Child Fetal Neonatal Ed. 2006 May;91(3):F213-20. PMC2672709.
- Gillies M, Bellomo R, Doolan L, Buxton B. Bench-to-bedside review: Inotropic drug therapy after adult cardiac surgery — a systematic literature review. Crit Care. 2005 Jun;9(3):266-79. PMC1175868.
- Hollenberg SM. Vasoactive drugs in circulatory shock. American journal of respiratory and critical care medicine. 183(7):847-55. 2011. [pubmed]
- Hollenberg SM. Inotrope and vasopressor therapy of septic shock. Critical care clinics. 25(4):781-802, ix. 2009. [pubmed]
- Jentzer JC, Coons JC, Link CB, Schmidhofer M. Pharmacotherapy update on the use of vasopressors and inotropes in the intensive care unit. Journal of cardiovascular pharmacology and therapeutics. 20(3):249-60. 2015. [pubmed]
- Overgaard CB, Dzavík V. Inotropes and vasopressors: review of physiology and clinical use in cardiovascular disease. Circulation. 2008 Sep 2;118(10):1047-56. PMID: 18765387. [Free Full Text]
- Senz A, Nunnink L. Review article: inotrope and vasopressor use in the emergency department. Emerg Med Australas. 2009 Oct;21(5):342-51. PMID: 19694785. [Free Full Text]
- Vasu TS, Cavallazzi R, Hirani A, Kaplan G, Leiby B, Marik PE. Norepinephrine or dopamine for septic shock: systematic review of randomized clinical trials. J Intensive Care Med. 2012 May-Jun;27(3):172-8. PMID: 21436167.
FOAM and web resources
- EMCRIT — Podcast 138 – Vasopressor Basics (2014)
- EMCRIT — Do phenylephrine and epinephrine require central access? (PulmCrit, 2016)
- EMCRIT — Peripheral vasopressor infusions and extravasation (PulmCrit, 2016)
- EMCRIT — Phenylephrine: an alternative viewpoint (PulmCrit, 2016)
- EMCRIT — Epinephrine challenge in sepsis (PulmCrit, 2016)

Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at the Alfred ICU in Melbourne. He is also a Clinical Adjunct Associate Professor at Monash University. He is a co-founder of the Australia and New Zealand Clinician Educator Network (ANZCEN) and is the Lead for the ANZCEN Clinician Educator Incubator programme. He is on the Board of Directors for the Intensive Care Foundation and is a First Part Examiner for the College of Intensive Care Medicine. He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives.
After finishing his medical degree at the University of Auckland, he continued post-graduate training in New Zealand as well as Australia’s Northern Territory, Perth and Melbourne. He has completed fellowship training in both intensive care medicine and emergency medicine, as well as post-graduate training in biochemistry, clinical toxicology, clinical epidemiology, and health professional education.
He is actively involved in in using translational simulation to improve patient care and the design of processes and systems at Alfred Health. He coordinates the Alfred ICU’s education and simulation programmes and runs the unit’s education website, INTENSIVE. He created the ‘Critically Ill Airway’ course and teaches on numerous courses around the world. He is one of the founders of the FOAM movement (Free Open-Access Medical education) and is co-creator of litfl.com, the RAGE podcast, the Resuscitology course, and the SMACC conference.
His one great achievement is being the father of three amazing children.
On Twitter, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC