Intercostal Drain Insertion
PREPARATION
- exclude contraindications
- consent
- IV access (analgesia, resuscitation medications or products)
- monitoring (SpO2, ECG, BP)
- confirm affected side (clinically + CXR)
- position: supine with arm abducted and hand under head
- local anaesthesia: lignocaine with adrenaline = 7mg/kg
EQUIPMENT
- chlorhexidine
- drape
- scalpel
- forceps
- clamp
- 2.0 suture
- gauze
- dressing
- 32 Fr drain (blood)
- underwater seal drainage system (primed)
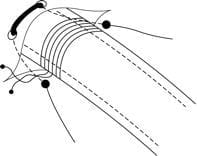
INSERTION
- full asepsis (G/G/H/M/C)
- landmarks = anterior to mid-axillary line, 5th IC space, nipple line (T4), palpate ribs and ICS
- 2-3cm transverse incision on top of rib
- blunt dissection down to pleura (just superior to rib -> avoid neurovascular structures)
- end point: pleural cavity (hiss or blood)
- sweep with finger
- insert clamped drain using curved forceps to guide in
- connect to UWSD
- check for drainage and respiratory swing
- suture
- sterile dressing
POST INSERTION
- CXR
- watch for complications:
-> not draining (check for kinking)
-> organ injury (lung, liver, spleen, heart, vessel) – careful insertion
-> blood loss– careful observation
-> surgical emphysema (small hole and good suturing)
->infection (sterile technique)
Features of a Pleural Drainage System
- modern drains incorporate three separate bottles into one unit
- bottle A = fluid trap
- bottle B = underwater seal drain
- bottle C = allows suction to be attached
Safety features:
1. first tube connecting drain to drainage bottles must be wide to decreased resistance
2. volume capacity of this tube should exceed ½ of patients maximum inspiratory volume (otherwise H2O may enter chest)
3. volume of H2O in bottle B should exceed ½ patients maximum inspiratory volume to prevent indrawing of air during inspiration
4. drain should always stay at least 45cm below patient (prevention of removed fluid or H2O refluxing into patient)
5. clamp drain when moving
6. H2O level above tube in bottle C determines the amount of suction applied before air drain through tube (safety suction limiting device)

Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC