Iron ingestion
Like all heavy metal exposures an acute ingestion results in gastrointestinal irritation and then dose-related systemic toxicity potentially leading to death. Iron takes hours to reach from the GI tract to the intracellular space. This gives us the opportunity to prevent further absorption in large overdoses with decontamination and chelation.
Toxic Mechanism:
Locally it is corrosive causing vomiting, diarrhoea, haematemasis and melaena with large GI fluid losses. Iron is a direct cellular toxin with major targets including the cardiovascular system and the liver. CNS toxicity results form the CVS instability and metabolic derangement. The coagulation cascaded is distributed and lactic acid forms from the liberation of hydrogen ions during the hydration of free ferric ions in the plasma.
Toxicokinetics:
- Absorption is normally finely regulated according to the body’s requirements, in overdose this mechanism is overwhelmed and bioavailability increases.
- Absorption of iron shifts intracellularly over a number of hours.
- Elimination is minimal in overdose.
Resuscitation:
- Hypovolaemia from GI losses:
- Give 10 – 20 ml/kg of IV crystalloid, if response is not adequate start noradrenaline [dose: 0.15mg/kg in 50ml D5W at 1-10ml/hr (0.05 – 0.5 mcg/kg/min)]. Ongoing fluid resuscitation is essential when there are ongoing losses and 3rd spacing.
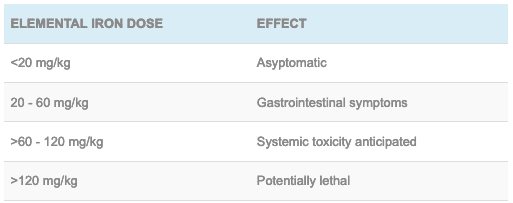
Risk Assessment
- Iron overdose can be lethal and is based on the elemental iron in each drug preparation. If in doubt always look up the drug, the elemental iron dose is always listed. Below is a calculator but beware errors can occur if you do not know if the sulphate is dry or not for example.
- [DDET + elemental iron calculations for ferrous or ferric salts] [table id=181 /] [/DDET].
- >60 mg/kg of elemental iron can potentially lead to systemic toxicity.
- The risk assessment can be refined by abdominal X-rays to count the number of tablets (if the preparation is radio-opaque) and a 4 – 6 hour post ingestion level.
- Systemic toxicity does not occur without GI symptoms.
- Those presenting with systemic features of toxicity have a poor prognosis.
- Children: The dose ingested is usually less than that expected to cause systemic toxicity (60mg/kg)
Clinical Features
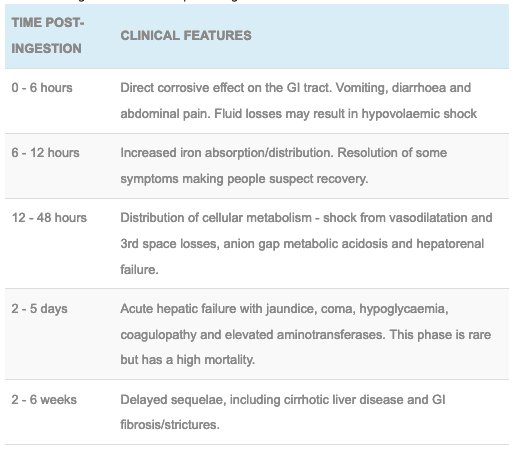
Classic stages of severe iron poisoning:
Note: sometimes these phases merge and it should be just thought of a gastrointestinal phase and a systemic toxicity phase.
Supportive Care
- Monitor fluid resuscitation and general supportive measure for any organ failure.
- Correct electrolyte abnormalities.
Investigations
- Screening: 12 lead ECG, BSL, Paracetamol level
- Specific:
- FBC, EUC, LFTs, ABG (anion gap metabolic acidosis)
- Chest and abdominal X-rays (can confirm and monitor ingestion but be careful, some preparations are not radio-opaque – this is not a rule out test).
- Serum iron concentration usually peaks at 4 – 6 hours post ingestion. Levels > 90 micromol/L (500 microgram/dL) are thought to be predictive of systemic toxicity.
- If iron levels are not available a fall in the bicarbonate in conjunction with worsening symptoms is a good surrogate marker for systemic toxicity.
Decontamination:
- Whole bowel irrigation with polyethylene glycol if the patient is cooperative and presents with >60mg/kg of elemental iron ingestion confirmed on X-ray.
- It requires one nurse – probably for the next 6 hours
- Place nasogastric tube and confirm with X-ray
- Administer PEG solution at 2L/hour by continuous infusion (children 25 ml/kg/hour)
- Given metoclopramide to reduce nausea and increase gastric emptying.
- Place the patient on a commode and continue until effluent is clear.
- Stop if there is abdominal distension or loss of bowel sounds.
- Serial abdominal X-rays can track the transit.
- If this is not possible it may be reasonable to remove the tablets via endoscope particularly when the ingestion maybe lethal.
Enhanced Elimination
- Not clinically useful
Antidotes
- Chelation is indicated when there is systemic toxicity (shock, metabolic acidosis, altered mental state) or a 4 – 6 hour iron level is >90 micromol/L (500 microgram/dL)
- Chelation with desferrioxamine is the agent of choice.
Disposition
- Children who have ingested <40 mg/kg can be managed at home if asymptomatic. Larger ingestions require evaluation. Those who are asymptomatic at 6 hours maybe discharged.
- Any adult who has ingested <60 mg/kg can be observed for 6 hours and if asymptomatic can be medically cleared.
- Symptomatic patients require admission and those with systemic toxicity require chelation and an ICU admission.
References and Additional Resources
Additional Resources:
- Tox conundrum 034 – The toddler with the Iron gut
- CCC – Iron overdose
References:
- Chyka PA, Butler AY. Assessment of acute iron poisoning by laboratory and clinical observations. American Journal of Emergency Medicine 1993: 11(2):99-103.
- Murray L et al. Toxicology Handbook 3rd Edition. Elsevier Australia 2015. ISBN 9780729542241
- Pearn J, Nixon J, Ansford A, et al. Accidental poisoning in childhood: five year urban population study with 15 year analysis of fatality. British Medical Journal 1984; 288:44-46.
- Singhi SC, Baranwal AK, Jayashree M. Acute iron poisoning: Clinical picture, intensive care needs and outcome. Indian Pediatrics 2003: 40(12):1177-1182.
- Tenenbein M. Benefits of parenteral deferoxamine for acute iron poisoning. Journal of Toxicology – Clinical Toxicology 1996; 34(5):485-489.

Toxicology Library
DRUGS and TOXICANTS
Dr Neil Long BMBS FACEM FRCEM FRCPC. Emergency Physician at Kelowna hospital, British Columbia. Loves the misery of alpine climbing and working in austere environments (namely tertiary trauma centres). Supporter of FOAMed, lifelong education and trying to find that elusive peak performance.