Jacques Lisfranc
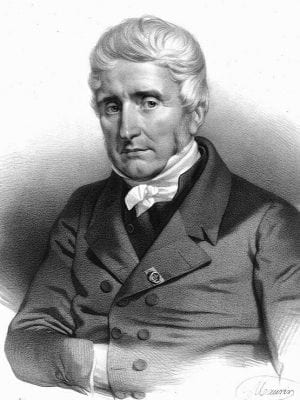
Jacques Lisfranc de Saint-Martin (1787 – 1847) was a French Surgeon.
Founder of a great number of surgical procedures including – surgical resection of the rectum in the treatment of rectal carcinoma (1826); lithotomy in women and the amputation of the cervix uteri
Performed and recorded many amputations most notably: désarticulation de l’épaule (1814); désarticulation tarso-métatarsienne: opération dite de Lisfranc (1815); désarticulation des métacarpes (1823), des phalanges des doigts (1823), de l’articulation coxofémorale (1823)
Eponymously affiliated with the Lisfranc joint/fracture/injury/amputation after he described an amputation method through the tarsometatarsal joints in 1815
Biography
- Born on April 12, 1787, in Saint Paul-en-Jarez, Loire. The descendant of three generations of surgeons: his father Jean-Baptiste (Saint-Paul); his grandfather Pierre (Royal College of Surgery of Lyon working in Pellussin); and his grandfather Pierre Cartal (Virieu)
- 1806-1813 Interne à l’Hôtel-Dieu de Lyon et de Paris and interne de Lyon. Trained under Jean-Marie Viricel (1773 – 1855) and Claude-Antoine Bouchet (1785 – 1839)
- 1811-1813 Posted to posted to Saint-Louis then to l’Hôtel-Dieu under Philippe-Jean Pelletan (1747-1829) and Guillaume Dupuytren (1777 – 1835); Medical doctorate defending thèse de médecine de Paris n° 135, describing Dupuytren’s operation for the removal of the lower jawbone.
- 1813 – Médecin aux armées (army surgeon) in Leipzig, the Battle of Hanau and then on to Metz by the end of the year. Reported to have performed myriad amputations and dis-articulations with great speed and accuracy during his 6 month tenure.
- 1814-1815 Famed or his ‘nouvelles méthodes opératoires‘ for the amputation of the arm ‘dans son articulation scapulo-humérale‘, and that of the partial amputation foot ‘dans son articulation tarsométatarsienne‘ which he presented to the institute.
- 1818 – Chirurgien du Bureau Central des Hôpitaux. Rapid rise in notoriety, commented on by his peers such as Louis Désiré Véron in 1853 “Le chirurgien Lisfranc fut l’ennemi et la caricature de Dupuytren“
- 1818-1822 Repeated failed applications for Chaires de Pathologie externe instead awarded to Marjolin, (1818) and Roux (1820). In 1822, when Frayssinous closed the Faculté de Paris, dismissing 11 professors, Lisfranc once agin applied to become Professeur à la Faculté.
- Lisfranc sought the assistance of Dupuytren who provided a long and detailed reference which described Lisfranc as “un chirurgien médiocre et bruyant, un boute-feu révolutionnaire, une sorte de Brutus solliciteur…“. The position was instead given to Bougon fresh from “sucé la blessure” of the assassinated Duc de Berry at the Opera.
- 1824 – Chirurgien en second à Saint-Louis, understudy to Jules Germain Cloquet (1790-1883)
- 1825 – Chief surgeon at l’Hôpital de la Pitié, Paris…despite the continued protestations of Dupuytren who maintained a policy to his senior students of “une entreprise odieuse d’écraser tout mérite naissant“.
- 1826 – Performed the first 5 operative resections for rectal carcinoma (20 years before the invention of anaesthetic…)
- 1835 – Lisfranc gave up on gaining a chair at la Faculté and turned his attention to the l’Institut instead. Again, after multiple failed attempts Lisfranc pushed for the Chair vacated by Dupuytren on his death.
Il mêlait le sarcasme et les explications cliniques, la maxime chirurgicale et l’anecdote égrillarde, tonnant sans trêve et sans dignité contre tous ceux qui lui portaient ombrage, en abandonnant le langage de la science pour le jargon des halles et des tréteaux.
Il parle en public et lors de ses cours sans cesse de “ces cochons de la Faculté“. Dès lors, on le dit atteint de “syncrasie colériconévralgique“
He combined sarcasm and clinical explanation; the surgical maxim and the lurid anecdote, thundering without truce and without dignity against all those who were shady, abandoning the language of the science for the jargon of halls and trestles.
In public and during his lectures, he inceasingly refers to “those pigs of the Faculty“. and was said to be suffering from “colériconeuralgique syncrasia“
- 1841-1847 Lisfranc gave up on public lectures and devoted himself to writing. First, De la clinique Chirurgicale de La Pitié (3 volumes from 1841-43); then his Traité de médecine opératoire (3 volumes 1846-47, the third volume finishing abruptly on page 332…).
- His final works were filled with controversy and rage towards Alfred Velpeau (1795 – 1867) another rival who was 2IC at la Pitié in 1830; author of the hugely successful surgical textbook Nouveaux Eléments de Médecine Opératoire in 1832; competitor in providing free public lectures and finally awarded chair of surgery at Larrey…ahead of Lisfranc.
- Died on May 12, 1847. On his tomb in Montparnasse, a quote from his book La Médecine Opératoire
Si la chirurgie est brillante quand elle opère, elle l’est encore bien davantage lorsque, sans faire couler de sang et sans mutilation, elle obtient la guérison des malades
Surgery is bright when operating but it is still brighter when there is no blood and mutilation and yet leads to the patient’s recovery
Eponyms
Lisfranc injury; ligament; joint; amputation… [opération de Lisfranc]
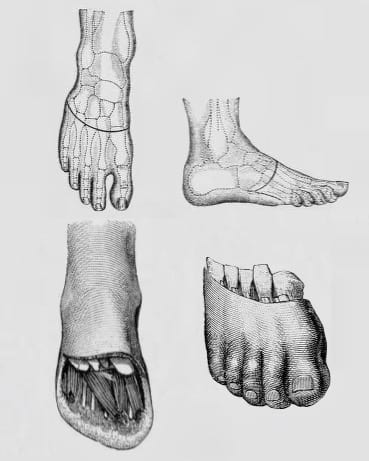
Like Chopart (with the midtarsal joint), Lisfranc is eponymously associated with his tarsometatarsal forefoot amputation; the joint disarticulated; and the associated fracture-dislocation.
- Lisfranc joint – the tarsometatarsal joint
- Lisfranc ligament – connects the superolateral surface of the medial cuneiform to the superomedial surface of the base of the second metatarsal
- Lisfranc amputation (tarsometatarsal disarticulation) – partial amputation of the foot at the tarsometatarsal joint. Famously performed by Lisfranc in less than a minute.
- Lisfranc injury – fracture and dislocation/subluxation of the tarsometatarsal joints with lateral displacement of the metatarsals
Lisfranc facilitated the trans-metatarsal amputation with what he termed his “master stroke” to transect the Lisfranc ligament:
Le couteau dans le dos s’appuie sur le tendon transversal du long péronier latéral, pénètre de la pointe, tranchant haut, dans l’interligne et coupe en se relevant le ligament inter-osseux par le coup de maître…
Malgré la supériorité vainement contestée de la méthode Chopart, les practiciens ont senti comme moi la nécessité de conserver plus de longueur au moignon.
Outre les muscles et les tendons qui fortifient la contiguité tarso-métatarsienne, elle possède des ligamens qui lui sont propres: l’articulation du second os du métatarse avec les cunéiformes en a trois pour sa face dorsale et trois pour la plantaire…
Telle que nous venons de la décrire, l’amputation partielle du pied dans l’articulation tarso-métatarsienne est terminée en moins d’une minute; or, il nous semble qu’on doit la préférer à celle de Chopart toutes les fois que le désordre des parties le permettre.
The knife in the back rests on the transverse tendon of the long lateral peroneus, penetrates from the point, sharp high, in the space and cut while raising the interosseous ligament with the masterstroke…
Despite the vainly contested superiority of the Chopart method, practicians such as I have felt the need to conserve more length in the stump.
Aside from the muscles and tendons which fortify the tarso-metatarsal joint, it also possesses ligaments of it’s own: the articulation of the second metatarsal bone with the cuneiforms has three (ligaments) on its dorsal and three on its plantar surface…
Such as we have described it, the partial amputation of the foot in the tarso-metatarsal articulation is completed in less than one minute; thus it would seem that one should prefer it to the Chopart method, whenever the derangement of the parts would permit.
Lisfranc’s description of amputation through the tarsal-metatarsal joints requires several pages to describe it, but it took only 1 minute for him to perform it — not too short a time for the unanesthetized patient
Cassebaum WH, 1963
Of note, Lisfranc never claimed the invention of this intervention stating:
Je n’ai jamais eu la prétention d’avoir imaginé l’amputation dans l’articulation tarso-métatarsienne: il m’appartient d’avoir le premier fait convenablement et rigoureusement l’anatomie chirurgicale de l’articulation du tarse avec le métatarse, et d’avoir décrit l’extirpation en masse de tous les métatarsiens avec assez de soin pour que l’opération soit devenue facile et promp.
I have never claimed to have imagined amputation in the tarso-metatarsal joint: it is up to me to have been the first to properly and rigorously perform the surgical anatomy of the tarsal joint with the metatarsus, and for having described the mass extirpation of all the metatarsals with enough care that the operation became easy and prompt.
Other eponyms
Lisfranc tubercle (1815)
Scalene tubercle on the first rib at the insertion of the scalenus anterior muscle
Châtaignier Lisfranc
Chestnut variety native to Saint-Paul-en-Jarez. Named in honor of the surgeon and his father surgeon
Key Medical Contributions
Other methods of disarticulation (1823)
In 1823 Lisfranc documented many and varied disarticulation methods and procedures including des métacarpes; des phalanges des doigts; and de l’articulation coxofémorale
Rectal carcinoma excision (1826)
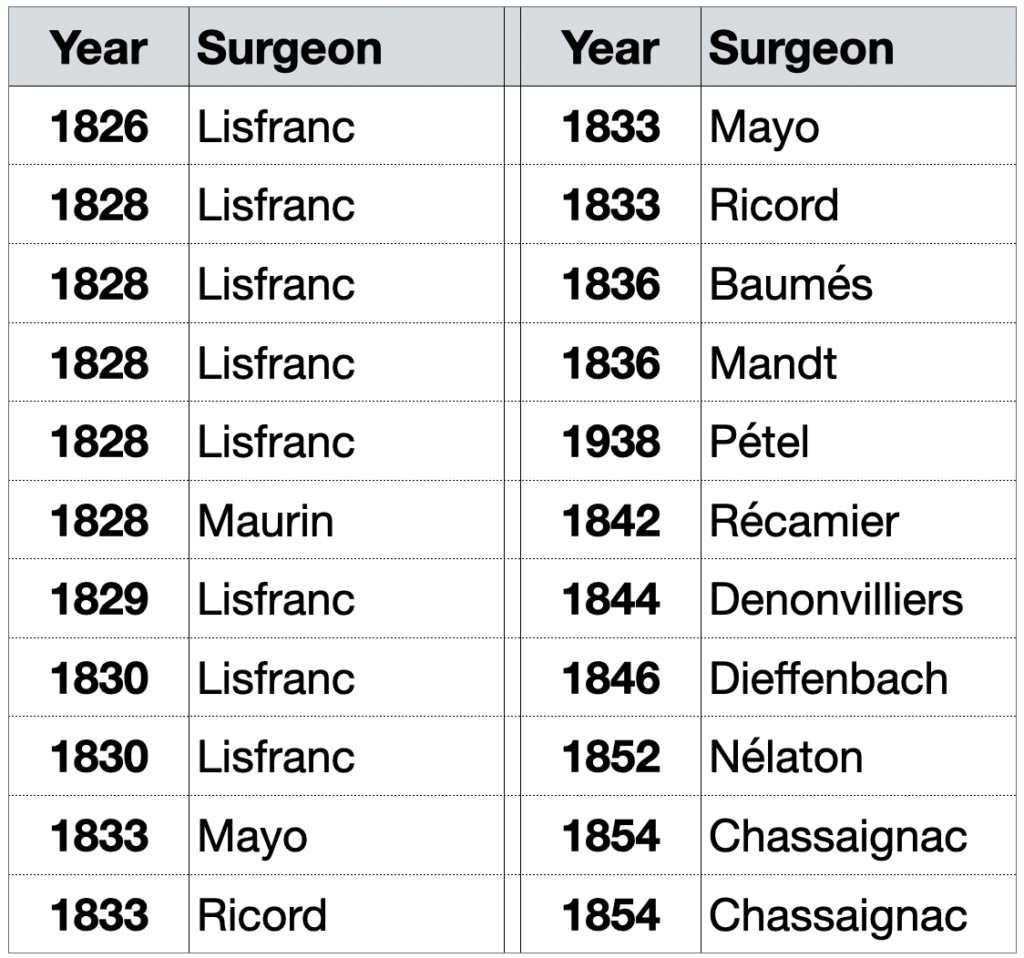
On March 24, 1830 Lisfranc presented to the Academy of Medicine his report on “excision of the lower part of the carcinomatous rectum“, an operation to remove up to 8 cm of the rectum. At the end of the report, published in 1833, Lisfranc indicates that he lost 3 out of 9 patients: two cases of local infection and one case of peritonitis verified by autopsy in subjects with already extensive cancers
Lisfranc’s operation is performed in two stages: lowering of the rectum, and resection tumor:
Le chirurgien fait, à un pouce environ de l’anus deux incisions semi-lunaires qui se réunissent en arrière et en avant du rectum ; on dissèque en dirigeant le bistouri perpendiculairement sur l’intestin qui est isolé de toutes parts : le doigt indicateur est introduit dans sa capacité ; il exerce sur lui des tractions qui les font saillir en bas.
The surgeon makes two semilunar incisions about an inch from the anus which meet behind and in front of the rectum; one dissects by directing the scalpel perpendicularly on the intestine which is isolated on all sides: the indicating finger is introduced in its capacity; he pulls down to allow them to protrude at the bottom.
He first performed successful excision of the rectum for uncomplicated cancer in 1826 at the Hôpital de la Pitié in Paris. He employed a perineal or posterior approach excising the infraperitoneal portion by pulling down and cutting a few centimetres of rectum.
Practiced after him by Velpeau, Chassaignac and Richet; perfected by Denonvilliers and Verneuil (with the resection of the coccyx); Lisfranc’s operation was the only one used for the next fifty years.
Controversies
Lisfranc, known for his booming voice and choleric lectures, referred to his teacher and colleague Baron Guillaume Dupuytren as “the brigand of l’Hotel Dieu.” Their rivalry was such that Dupuytren prevented Lisfranc from becoming a professor of the Faculty of Medicine of Paris. Lisfranc was an excellent surgeon, but equally as polemic as Dupuytren and not a nice chap by all accounts…
Jacques Lisfranc of Saint-Martin was born on April 12, 1787 ( not on April 2, 1790 as claimed by most) – Review the baptism certificate and Plaque [Fischer LP 2005]
Major Publications
- Lisfranc J, Champesme J. Mémoire lu à l’Institut le 21 novembre 1814, sur un nouveau procédé pour l’amputation du bras dans l’article applicable à la résection de la tète de cet os. Paris, 1815 [Lisfranc arm amputation at the shoulder]
- Lisfranc J. Nouvelle méthode opératoire pour l’amputation partielle du pied de son articulation tarsométatarsienne. Mémoire présenté à la première classe de l’Institut. 1815. [Lisfranc amputation Tarso-metatarsal joint]
- Lisfranc J. Mémoire sur un nouveau procédé pour l’amputation dans les articulations des phalanges
- Archives générales de médecine. 1823.
- Lisfranc J. Memoire des méthodes et des procédés nouveaux pour pratiquer l’amputation dans l’articulation scapulo-humérale. Archives générales de médecine. 1823; II: 28-30
- Lisfranc J. Mémoire sur un nouveau procédé opératoire pour pratiquer l’amputation dans l’articulation coxo-fémorale. Archives générales de médecine. 1823; II: 161-188
- Lisfranc J. Nouvelle methode operatoire pour l’amputation partielle du pied. Archives générales de médecine. 1823; III: 52-67
- Lisfranc J. Mémoire sur de nouvelles applications du stéthoscope de M. le professeur Laënnec. 1823.
- Lisfranc J. Considérations anatomiques, physiologiques et pathologiques sur la luette. 1823
- Lisfranc J. Mémoire sur une nouvelle méthode de pratiquer l’opération de la taille chez la femme. 1823.
- Lisfranc J. Mémoire sur le traitement des affections cancéreuses du col de l’utérus en particulier, et sur son amputation (publié par Avenel A). Revue médicale, 1828; 3: 5-37 [amputation of the cervix uteri]
- Lisfranc J. Mémoire sur les cancers superficiels qu’on croyait profonds, et observations. Mémoires de l’Académie de Médecine. 1833; III: 20-28
- Lisfranc J. Mémoire sur l’excision de la partie inférieure du rectum devenu carcinomateux. Mémoires de l’Académie de Médecine. 1833; III: 291-302 [rectal carcinoma excision]
- Lisfranc J. D’une tumeur particulière de l’utérus. Gazette médicale de Paris 1834; 2(2): 149-153
- Lisfranc J. Clinique chirurgicale de l’Hôpital de la Pitié. Vol I, Vol II, Vol III. 1841
- Lisfranc J. Précis de médecine opératoire. Vol I, Vol II, Vol III. 1846
- Lisfranc J. Diseases of the uterus, a series of clinical lectures. 1846
References
Biography
- The Duchess of Berry. The Sydney Gazette and New South Wales Advertiser, 1833: 4
- Véron LD. Mémoires d’un bourgeois de Paris. 1853; 1: 331
- Rochard J. Histoire de la chirurgie française au XIXème siècle. 1875: 172-176
- Fischer LP. Jacques Lisfranc de Saint-Martin (1787-1847). Hist Sci Med. 2005; 39(1): 17-34.[PDF]
- Jacques Lisfranc of Saint-Martin. Cimetière du Sud, dit du Montparnasse. Napoleon Monuments.
- Bibliography. Lisfranc M (Jacques) 1790-1847. WorldCat Identities
Eponymous terms
- Notice analytique sur les travaux de Lisfranc. 1834. Cote: 110133 vol. C n° 7. Bibliothèque interuniversitaire de santé (Paris)
- Garrè C, Borchard A. Amputation und Exartikulationen. Lehrbuch der Chirurgie, 1922: 693-695
- Mettler CC. History of medicine a correlative text, arranged according to subjects. 1947:
- Cassebaum WH. Lisfranc fracture-dislocations. Clin Orthop Relat Res. 1963;30:116-29.
- Christie J, Clowes CB, Lamb DW. Amputations through the middle part of the foot. J Bone Joint Surg Br. 1980; 62-B(4): 473-4. [PDF]
- Viso L, Uriach J. The first twenty operations for rectal cancer. Int J Colorectal Dis. 1995; 10(3): 167-8.
Resident medical officer in emergency medicine MB ChB (Uni. Dundee) MRCS Ed. Avid traveller, yoga teacher, polylinguist with a passion for discovering cultures.


BRILLANT AS USUAL