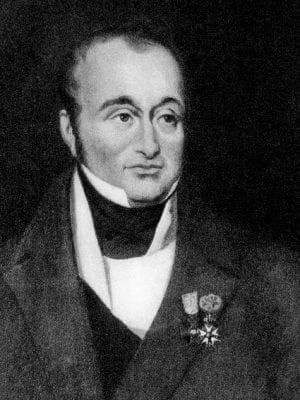
Guillaume Dupuytren
Baron Guillaume Dupuytren (1777-1835) was a French Surgeon.
Dupuytren was a center of controversy during his life. About no other surgeon have so many violently opposing opinions been expressed by his associates and perpetuated by his biographers. In a fiercely competitive system he rose in 20 years from the position of prosector of anatomy to become Chief Surgeon of the l’Hôtel-Dieu. Pompous, polemic and forever in conflict with his peers
He was without doubt the greatest French surgeon since Paré. His greatest contributions were in the field of surgical pathology and his eponym has been applied to at least twelve diseases, operations, or instruments, the most widely used being Dupuytren contracture (disease)
Born in poverty he purportedly became the richest physician of his time. Dupuytren was reputed to have seen up to 10,000 patients a year and amassed such a fortune he was able to offer Charles X a million francs to tide him over when he was de-throned (Equivalent to $5.5million USD in 2015)
Biography
- Born on October 5, 1777 in Pierre-Buffière, France
- 1789 – Taken by cavalry officer to Paris. Studied at College de La March
- 1795 – Prosector at école de médecine, Paris. Struggled against poverty but remained in Paris against the wishes of his parents
- 1801 – Le Chef des travaux anatomiques de la faculté de médecine. Laennec and Cruveilhier were his pupils at this time
- 1804 – Surgeon of the second class at l’Hôtel-Dieu – obtained exemption from conscription to the army on the plea of the faculty of école de médecine
- 1808 – Adjunct Surgeon, l’Hôtel-Dieu under Philippe-Jean Pelletan. Dupuytren severely criticized the diagnoses of his chief and in turn was mercilessly berated for his opinions, manners and attitudes. Percy termed him “le premier des chirurgiens et le dernier des hommes” [First amongst surgeons and last amongst men]
- 1812 – MD, defended Thesis on Lithotomie; Professor of Operative Medicine, l’Hôtel-Dieu; chair of of operative medicine at l’école de médecine; teacher of Jacques Lisfranc (1787-1847)
- 1816 – Created a Baron and awarded the Ordre de Saint-Michel; personal surgeon to Louis XVIII
- 1821 – Surgeon to Charles X of France
- 1833 – While walking to his work at the l’Hôtel-Dieu, was seized with an attack of apoplexy (hemiparesis and a facial palsy). He was forced into early retirement and travelled to Italy with acclaim at each place he visited. His health did not recover and he returned to Paris.
- Died on February 8, 1835 aged 58. Left 200,000 francs to medicine – used to create a pathologic museum – the Musée Dupuytren, which opened in November 1835i n Paris
The late M. Dupuytren in his last illness had effusion into the chest consequent on a pleurisy. He was at first disposed to have himself tapped for it; he changed his mind, and observed, “Je préfère mourir par la main de Dieu que par celle des hommes [I would rather die by the hand of God than of man]”
Husson, 1835
The surgeon
Dupuytren was efficient, rigid and unvaried in his routine. He was a brilliant diagnostician, always ready with the essential question in the history, keenly aware of the physical signs of disease. Dupuytren attracted large numbers of students to his ward rounds and lectures. As many as 1,200 students, an incredible number, attended some of his lectures on hernia.
I saw him…a square solid man with a high-domed head, oracular in his utterance, indifferent to those around him, sometimes, it was said, very rough with them. He spoke in low even tones, with a quiet fluency, and was listened to with that hush of rapt attention which I have hardly seen in any circle of listeners…he dominated those around him in a remarkable manner. The personal presence of some men carries command with it, and their accents silence the crowd around them, when the same words from other lips might fall comparatively unheeded.
Oliver Wendell Holmes 1896: 428
With his own record librarian, he kept meticulous records of the history, physical findings, course of the disease, and the description of the surgical or autopsy specimens. This allowed him to accurately evaluate his diagnostic and treatment processes.
For example, his 6 degree classification of burns was based on 50 patients attending l’Hôtel-Dieu in 1828. Patients were classified by age, sex, size and location of the burned area, and cause of death (mortality rate 13.6%). Such numerical and statistical data gives his writing a very modern air when compared with that of most of his contemporaries.
Dupuytren was not always right, unfortunately, and his incorrect opinions were supported by the same weight of authority as his correct ones. He did not grasp the concept of acute appendicitis teaching that the acute suppurative processes arose from the caecum, despite fellow surgeons such as Meijer reporting the appendix as the seat of the disease. Dupuytren’s insistance on the importance of the caecum retarded the general recognition of appendicitis as a disease for many years.
If he was excelled in a few particulars by some surgeons, – if, for example, as we admit, Roux was quicker and more dexterous at an operation, – Dessault more brilliant as a professor, – Boyer more prudent and humane, and Marjolin more profound, – there was none who could compare with him for imperturbability of mind in the midst of accidents or untoward circumstances, – none whose eye was more certain, or whose hand was more firm.
Editorial, Boston Med Surg J 1835
Of note, following his death in 1835, the positions held by Dupuytren were passed on, not to one man, but to three; Roux taking his service at the l’Hôtel-Dieu, Sanson his chair of clinical surgery, and Breschet his chair at the Académie de médecine.
Of the many crimes of which he was accused, no one ever suggested that he put his private interest above that of the meanest of his patients. His funeral cortege was interrupted as it made its way to the cemetery by crowds of workmen who took the coffin on their shoulders and bore it part of the distance.
Medical Eponyms
Dupuytren fracture (1819)
archaic: fracture distal fibula; damage to tibio-fibular ligaments and deltoid ligament; lateral displacement of the talus +/- fracture of the medial malleolus [similar to Pott’s fracture].
Dupuytren outlined the fracture in a long and learned treatise of 212 pages including a description of experimental fractures produced in cadavers to elucidate the mechanism of injury.
Two varieties were distinguished:
- High Dupuytren: fracture of the fibula 2-3 inches above the syndesmosis; due to external rotation fracture or flexion-rotation strain
- Low Dupuytren: fracture of the fibula within an inch of the syndesmosis; in which abduction violence usually predominates
Dupuytren was a strong advocate of the practice of Sir Percivall Pott (1714 – 1788), who used the semi-flexed position in treating fractures of the extremities in order to obtain the maximum degree of muscular relaxation. This was contrary to the method of treating fractures in extension then well established in France.
Dupuytren outlined an a new method of treating these fractures (evaluated in 207 patients with the injury) – the Dupuytren splint consisting of:
- a wedge-shaped cushion about two-thirds filled with bran or cotton and of sufficient length to extend from the internal malleolus to the knee,
- a wooden splint about 2 feet long and 3 inches wide, and
- 2 roller bandages 4 or 5 yards long.
The fracture was reduced by manipulation with inversion of the foot. The wedge-shaped cushion, base downward, was applied to the inner side of the leg. The splint was then applied to the cushion and extended below the sole of the foot. These were then firmly held in place by the roller bandages applied from just below the knee to a short distance above the fracture, and thence around the foot and instep in a figure-of-eight to maintain the inversion of the foot
- Dupuytren G. Mémoire sur la fracture de l’extrémité inférieure du péroné, les luxations et les accidens qui en sont la suite. Annuaire médico-chirurgical des Hopitaux et Hospices civils de Paris 1819; 1: 1-212 [Of fractures of the lower extremity of the fibula and luxations of the foot, Med Classics 1939; 4: 151-172]
- Dupuytren G. On fractures of the fibula. Quarterly journal of foreign medicine and surgery. 1821; 3: 177-238
Dupuytren contracture (1831) A gradual thickening and tightening of the fascia (fibrous tissues layer) under the skin of the palm and fingers in the hand.
Dupuytren Enterotome (1816) Dupuytren invented an enterotome to perform his operation for artificial anus. He had tried many methods of creating colostomies, and after a large number of experiments on dogs finally developed his enterotome.
The enterotome was first used on a patient in 1816. By his 1928 publication, Dupuytren was able to report upon its use in 41 patients. In 29 of these there was a complete cure; in 9, partial success with a residual fistula; and, in 3 death from peritonitis.
- Dupuytren G. Mémoire sur une méthode nouvelle pour traiter les anus accidentels. Mémoires de l’Académie de médecine, 1828; 1: 259-316, Paris, 1828.
- Dupuytren’s enterotome for artificial anus. Nouveaux élements de médecine opératoire. 1832: Plate XIV(8)
- Buchanan G. Case of Artificial Anus, Successfully Treated by Dupuytren’s Enterotome. Edinb Med J. 1869; 14(10): 865-869
Dupuytren’s classification of burns (1828) Ambroise Paré (1510-1590) described different degrees of burns in the 1500s; Fabricius Hildanus described three degrees of burns in 1607; Heister (1724) and Richter (1788) classified burns into four degrees. Dupuytren analysed 50 burns patients in 1828 and classified the 6 degrees of burns and their management.
Brûlures au premier degré (rubéfaction); deuxième degré (vésication); troisième degré (escarres du corps muqueux); quatrième degré (escarres de l’épaisseur de la peau); cinquième degré (escarres jusqu’aux os); sixième degré (combustion totale d’une partie)
Burns in the first degree (erythema); second degree (skin inflammation with epidermal detachment); third degree (eschars of the rete mucosum); fourth degree (eschars of the skin); fifth degree (eschars of the bone); sixth degree (destruction of a part)
Of Burns, In: Clinical lectures on surgery 1832; (1)XVII: 229-280
Dupuytren-Nélaton disease [Nélaton’s tumor] central tumor of bone.
- Dupuytren G. Des kystes qui se dévelop dans l’épaisser des os, et de leurs différentes espéces. In: Leçons orales de clinique chirurgicale faites à l’Hôtel-Dieu de Paris. 1832;(2):129-148.
- Nélaton A. Des kystes des os. Élements de pathologie chriurgicale. 1844; 2(XXVII): 46-52
Other eponyms
- Dupuytren operation / amputation: a method of removing the arm at the shoulder joint; also termed Lisfranc amputation.
- Dupuytren abscess: Abscess of the right iliac fossa. [Abcès développé dans le petit bassin. Revue médicale française et étrangère, 1829; 1: 367-368]
Key medical contributions
1812 – First to successfully excise the lower jaw
- Dupuytren G. Observation sur une résection de la mâchoire inférieure. Journal universal des sciences médicales. 1820; 19: 77-98
- Dupuytren G. De l’amputation et de la résection de la mâchoire inférieure. Leçons orales, 1829; 2: 410-453
1815 – Successful ligation of the external iliac artery
- Dupuytren G. Observation sur un cas de ligature de l’artère iliaque externe. Répertoire général d’anatomie et de physiologie pathologiques 1826; 2: 230-250
1818 – Dupuytren was the first successfully to treat aneurysm by compression.
M.Dupuytren a présenté à la Société un malade guéri en quinze jours de temps, d’un anéurisme å l’artère poplitée, par une compression exercée sur la partie inférieure de l’artère fémorale, à l’aide d’un compresseur formé par deux tiers de cercle supportant à l’une des extrémités une pelote permanente, et à l’autre une pelote mobile. Ce malade est le second que M. Dupuytren a guéri par ce moyen.
Dupuytren. Anéurisme à l’artère poplitée par la compression. Bulletins de la faculté de médecine de Paris 1818; 6: 242
Mr Dupuytren presented to the Society a patient cured in two weeks time, of an aneurism in the popliteal artery, by a compression exerted on the lower part of the femoral artery, using a compressor formed by two-thirds of a circle supporting at one end a permanent ball, and at the other a movable ball. This patient is the second that Mr Dupuytren cured by this means
Dupuytren. Anéurisme à l’artère poplitée par la compression. Bulletins de la faculté de médecine de Paris 1818; 6: 242
1819 – First successful ligation of the subclavian artery.
- Dupuytren G. Account of the tying of the subclavian artery. Edinburgh Medical Journal 1819; 15: 476
1822 – Dupuytren was the first to treat chronic (3 years) wry neck by subcutaneous section of the sternomastoid muscle in a 10 year old girl on January 16,1822
- Dupuytren G. De la section du sterno-cléido-mastoidien pour guérir le torticolis ancien. In: Leçons orales. 1839; 3(XII): 454-461
- Averill C. Wry neck, the operation as performed by M. Dupuytren. In: A short treatise on operative surgery. 1823: 61-64
1826 – Dupuytren provided the first clear pathological description of congenital dislocation of the hip (CDH). He distinguished CDH from deformities secondary to tuberculosis and pyarthrotic disease of the hip joint. Dupuytren examined at least 30 patients with this condition, 26 women and 4 men and intimated the familial nature of the condition citing a family of 3 generations with the condition
- Dupuytren G. Mémoire sur un déplacement originel ou congénital de la tête des fémurs. Répertoire général d’anatomie et de physiologie pathologiques 1826; 2: 82-93
1832 – Dupuytren was the first to differentiate between provisional callus, forming quickly during the first month of healing, and definitive callus, which produced final solid union of the fracture after many months.
Controversies
Not a very nice chap really: Lisfranc referred to Dupuytren as “the brigand of the Hôtel Dieu” and Pierre-François Percy (1754-1825) referred to him as “first among surgeons, last among men”
The contemplation of his features left a “je-ne-sçai-quoi” impression on the feelings even of the most acute physiognomists, – half pleasurable and half dissatisfied, – a sensation at once of admiration and dislike, for which it was found impossible to account.
Editorial, Boston Med Surg J 1835
The Lancet reflected on his life from an academic point of view “Regarding surgery in the true sense, we hesitate not to place the late Baron Dupuytren at the head of European surgery“
Dupuytren felt conscious of the superiority which he so fully possessed; and to justify his pretensions, he sacrificed all the pleasures and comforts of private life, and condemned himself, as we have heard him say, “to lead the life of a dog.” “Above all things avoid being an insignificant man ” [ce qu’il faut craindre avant tout, c’est d’etre un homme mediocre], was one of his favorite maxims, and to escape the chance of a humiliating mediocrity he devoted every energy of his mind, succeeding lo the utmost verge of his resolve, but not without most bitterly experiencing the stings of envy and calumny, nor without nourishing an implacable hatred against the authors of reports which a man of less susceptibility would have treated with deserved contempt.
Editorial, Boston Med Surg J 1835
Dupuytren argued with pretty much everybody. One example is over the ‘original‘ description of melanoma. He fought publicly with one of his former pupils René Laennec with argument and counter-argument being published as multiple articles within the same journal.
Laennec published ‘Sur les maelanoses‘ – but Dupuytren felt his article failed to give him enough credit so published ‘Anatomie pathologique‘ in the same journal. When Laennec retorted with ‘Note sur l’anatomie pathologique‘ in the Journal de médecine, chirurgie, pharmacie…then Dupuytren responded, again in the same journal with Observations and Nouvelles Observations…
Major Publications
- Dupuytren G. Propostions sur quelques points d’anatomie, de physiologie, et d’anatomie pathologique. 1803
- Dupuytren G. Lithotomie: Thèse soutenue publiquement dans l’amphithéâtre de la Faculté de médecine de Paris. 1812
- Dupuytren G. De la rétraction des doigts par suite d’une rétraction de l’aponévrose palmaire. Paris, 1831; 2s(5): 352-365.
- Dupuytren G. Lettre et leçon de M. le professeur Dupuytren, sur le siège, la nature et le traitement du choléra-morbus. 1832
- Dupuytren G. Permanent retraction of the fingers, produced by affection of the palmar fascia. Lancet, 1833-1834; 2: 222-225. [English translation and reprint in Medical Classics, 1939; 4: 142-150]
- Dupuytren G. Leçons orales de clinique chirurgicale faites à l’Hôtel-Dieu de Paris 1832. [Tome II][Tome III][Tome IV] [English translation: Clinical lectures on surgery: delivered at Hotel Dieu]
- Dupuytren G. Traité, théorique et pratique, des blessures par armes de guerre, rédigé d’après les leçons cliniques de M. le baron Dupuytren. 1834
References
Biography
- Jean Louis Hippolyte Peisse. Sketches of the character and writings of eminent living surgeons and physicians of Paris. 1831: 1-22 [English translation; Elisha Bartlett]
- Editorial. Memoir of Dupuytren, Late Surgeon of the Hotel Dieu, Boston Med Surg J 1835; 12:165-171
- Pariset E. Eloge upon Baron G. Dupuytren. 1837
- Muséum d’anatomie pathologique de la Faculté de médecine de Paris, Musée Dupuytren. 1842
- Malgaigne JF. Notice sur Dupuytren. 1856
- Gaillard FL. Dupuytren. 1865
- Faure J-L. Dupuytren. 1935
- Editorial. Guillaume Dupuytren (1777-1835) the brigand of Hôtel-Dieu. JAMA. 1964;189(6):509-510
- Fresquet JL. Guillaume Dupuytren (1777-1835) Historia de la Medicina.
- Bibliography. Dupuytren, Guillaume 1777-1835. WorldCat Identities
Eponymous terms
- Dupuytren Enterotome. Modern surgical instruments chiefly of France and Germany. 1844: Plate V(XI)
- Peltier LF. Guillaume Dupuytren and Dupuytren’s fracture. Surgery. 1958 May;43(5):868-874.
- Peltier LR. Six eponymic fractures. Bull Med Libr Assoc. 1960 Jul;48:345-351
- Beighton P, Beighton G. Guillaume Dupuytren. In: The Man Behind the Syndrome. 1986: 46-48
Resident medical officer in emergency medicine MB ChB (Uni. Dundee) MRCS Ed. Avid traveller, yoga teacher, polylinguist with a passion for discovering cultures.