John B. Murphy
John Benjamin Murphy (1857-1916) was an American physician and abdominal surgeon
Arguably the first surgeon to perform a biliary tract endoscopy and first to perform femoral artery anastomosis after gunshot injury. Murphy described his clinical experience and experimentation with injured blood vessels in resection of arteries and veins injured in continuity– end-to-end suture (1897)
Multiple eponyms named after him including Murphy’s Sign (1903) for clinical diagnosis of cholecystitis describing a hooking technique rather than an anterior subcostal approach to detect gallbladder hypersensitivity. Notable advocate for early surgical intervention in appendicitis
William J. Mayo described him as “the surgical genius of our generation”; and Loyal Davis termed the fabled surgeon “extraordinary” and the “stormy petrel of American surgery”
Biography
- Born on December 21, 1857 in Appleton, Wisconsin on 21 .
- 1879 – Doctorate from Rush Medical College
- 1882 – Worked closely with Theodor Billroth (1829-1894) (famous for the Billroth Gastrectomy) in Vienna
- 1890 – Professor of Surgery at Rush Medical College
- 1892 – Professor of Clinical Surgery at the College of Physicians and Surgeons
- 1895 – Surgeon in Chief at Mercy Hospital
- 1901 – Professor of Surgery at Northwestern University Medical School
- 1912 – Performed the first biliary tract endoscopy (this claim is argued)
- Died 1916
Medical Eponyms
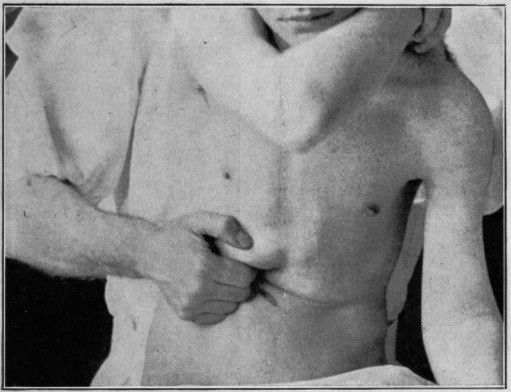
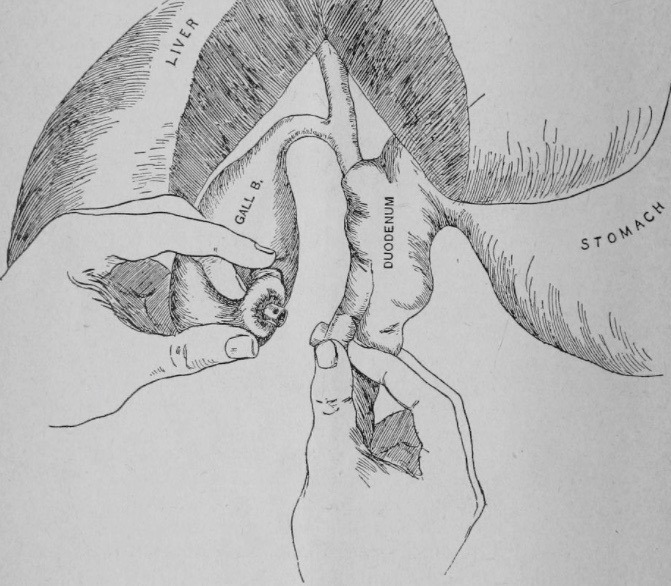
Murphy’s Sign (1903)
Pain elicited in patients with acute cholecystitis by asking the patient to take in and hold a deep breath while palpating the subcostal region
The most characteristic and constant sign of gall-bladder hypersensitiveness is the inability of the patient to take a full, deep inspiration, when the physician’s fingers are hooked up deep beneath the right costal arch below the hepatic margin. The diaphragm forces the liver down until the sensitive gall-bladder reaches the examining fingers, when the inspiration suddenly ceases as though it had been shut off. I have never found, this sign absent in a calculous or infectious case of gall-bladder, or duct disease.
Murphy 1903: 827-828
Murphy’s Percussion Test:
Murphy described a perpendicular percussion technique for evaluation of the inflamed gallbladder
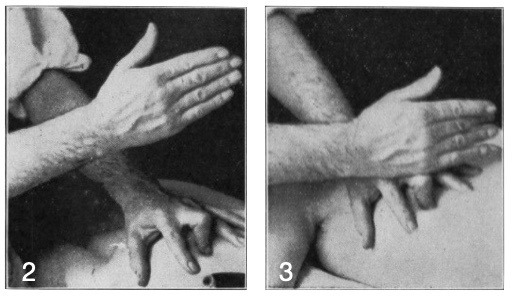
Fig 2; Shows the hand elevated, with the middle finger flexed perpendicularly at the tip of the ninth costal cartilage.
Fig 3; Shows the finger struck with the right hand when the patient is in deep inspiration. This causes great pain if the gall-bladder is distended or inflamed. Murphy 1910
Murphy’s Punch Test
Pain upon percussion / punch tenderness at the costo-vertebral angle indicative of perinephric abscess, pyelonephritis, renal stone or haemorrhagic fever with renal syndrome
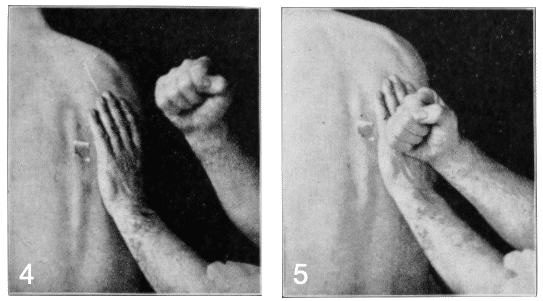
Fig 4; Shows the palm of the left hand pressed firmly over the right renal zone and the right elevated to make the stroke.
Fig 5; The stroke completed. When the kidney is actually inflamed, the pelvis distended or the ureters obstructed, there is great pain elicited by the blow: if the lesion is in the appendix or in the gall-bladder there is no pain produced. Murphy 1910
Murphy’s sequence [Murphy’s Triad, Murphy’s Quadrad]
1895 – Murphy initially presented a quadrad of signs in his report and analysis of one hundred and forty-one histories and laparotomies
Upon what cases should we operate? Upon every case of appendicitis, or better, upon every case where we have present the four cardinal symptoms: 1. Sudden attack of pain over appendix. 2. Always nausea, frequently vomiting. 3. Elevation of temperature, and 4. Local tenderness in the position occupied by the appendix
Murphy 1895: 14-15
1904 – Murphy recognized an ordered sequence of signs and symptoms in his analysis of Two Thousand Operations for Appendicitis and Deductions from His Personal Experience. He included low grade fever in the sequence but with the proviso that a raised temperature at any given stage of the attack is not invariable and is not an essential feature in establishing a diagnosis. Murphy’s sequence (quadrad) is often shortened to a triad of signs and symptoms excluding fever.
The symptoms in the order of their occurrence may be mentioned as: first, pain in the abdomen, sudden and severe, followed by (second) nausea or vomiting, even within a few hours, most commonly between three and four hours after the onset of pain; third, general abdominal sensitiveness most marked in the right side, or more particularly over the appendix; fourth, elevation of temperature, beginning from two to twenty-four hours after the onset of pain…The symptoms occur almost without exception in the above order, and when that order varies I always question the diagnosis. If the nausea and vomiting or temperature precede the pain I feel certain that the case is not one of appendicitis
Murphy 1904: 190
Murphy Button [Anastomosis Button] (1894)
Murphy’s preferred cholecystoenterostomy over cholecystostomy or cholecystectomy for the operative management of cholecystic disease. Murphy created a surgical device to create the anastomosis between the gallbladder and the duodenum. The ‘anastomosis button’ was a hollow-cored spherical device divisible into two hemispheres, over which the purse-stringed segments to be anastomosed could be affixed.
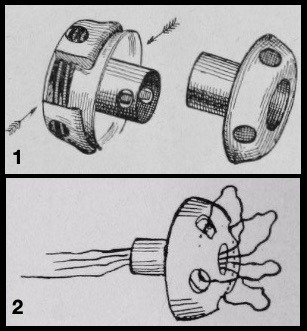
1. Anastomosis Button
2. Half button threaded for introduction into gallbladder
The two halves of the brass ‘anastomosis button,’ were joined and then locked together, facilitating rapid apposition of the two segments. The button was then ‘passed’ a few weeks following insertion, leaving the anastomosis intact.
Murphy performed first cholecystoenterostomy on a 35-year-old, severely jaundiced woman, joining the gallbladder with the jejeunum by means of the button. The gallstones were not removed. ‘Time from opening of the peritoneum until the closing of same, eleven minutes.’ reducing the standard operating time for the anastomosis tenfold. The Mayo brothers, William and Charles, visited Murphy’s clinic and adopted the ‘Murphy Button’ for use in the Mayo Clinic, where it remained in common use until 1935.
Other Medical Eponyms
- Murphy-Lane bone skid – Surgical instrument used primarily for femoral head procedures
- Murphy’s Drip – The administration of rectal fluid by proctoclysis in patients with peritonitis
Key Medical Attributions
1912 – Described the first biliary tract endoscopy by inserting a cystoscope into a cholecystostomy drainage tract, passing a hook through the cystoscope and removing a residual stone. He describes the procedure:
It showed that a small stone was present in the hour-glass contraction zone, where the large stone had formerly been lodged. The cystoscope was pressed on this to the round ligament; a hook passed through the cystoscope to the stone. The stone was rotated and jammed against the edge of the cystoscope, and by this means it was extracted for its position.
Cholelithiasis. Surgical Clinics of JB Murphy 1912
Controversies
The offspring of humble Irish immigrants born in a log cabin on a farm in Appleton, Wisconsin, he was originally named simply John Murphy. As every other child in his school had a middle name, he added a ‘B’ to his name, later this became Benjamin.
JB Murphy is most probably the source of the quote most commonly attributed to Osler
Dr. NC. Gilbert tells how Dr. Murphy used to shake his finger in the students’ faces and say in his shrill voice, “Listen, listen to the patient’s story! He is telling you the diagnosis.”
Gilbert NC. JAMA 1939
Anecdotally, 2 days before his death he correctly predicted his own autopsy findings: ‘I think the necropsy will show plaques in my aorta‘
Major Publications
- Murphy, JB. Early treatment of perityphlitis. Western Medical Reporter 1889; 11: 282–291
- Murphy JB. Cholecysto-intestinal, gastro-intestinal, entero-intestinal anastomosis, and approximation without sutures. Medical Record (New York) 1892; 42(24): 665–676
- Murphy, JB. Operative surgery of the gall tracts with original report of twenty successful cholecystenterostomies by means of the anastomosis button. 1894 [Murphy’s button]
- Murphy JB. Appendicitis: with original report and analysis of one hundred and forty-one histories and laparotomies for that disease under personal observation. 1895
- Murphy JB. Surgical clinic and demonstration. 1895
- Murphy JB. Traumatisms of the urinary tract 1895
- Murphy, JB. Fibromyoma complicating pregnancy; Fibroma of vaginal wall. American Medical Association Press. 1896
- Murphy JB. Ileus. American Medical Association Press. 1895
- Murphy JB. Resection of arteries and veins injured in continuity– end-to-end suture: experimental and clinical research New York: Publishers Printing Co. 1897
- Murphy JB. The diagnosis of Gall-stones. The Medical News (London). 1903; 82(2): 825-883 [Murphy’s sign]
- Murphy JB. Two Thousand Operations for Appendicitis and Deductions from His Personal Experience. Am J Med Sci 1904; 128: 187–211
- Murphy JB. Neurological Surgery. 1907
- Murphy JB. Gallstone disease and its relation to intestinal obstruction. Illinois Medical Journal. 1910; 18: 272-280
- Murphy, JB. Cholelithiasis. The Surgical Clinics of John B. Murphy, 1912; 1(1): 417-428
- Murphy JB. 5 diagnostic methods of John B, Murphy. The Surgical Clinics of John B. Murphy, 1912; 1(1): 459-466 [Murphy’s punch test; Murphy’s sign]
References
Biography
- Abt, AF. John Benjamin Murphy, Chicago Surgeon. JAMA. 1968; 204(13): 1198
- Schmitz, RL. Oh, TT. The Remarkable Surgical Practice of John Benjamin Murphy. University of Illinois Press 1993
- Musana, K. John Benjamin Murphy (1857 – 1916). Clin Med Res. 2005; 3(2): 110–112.
- Morgenstern L. J. B. Murphy, M.D. Surgical Endoscopy, 1998; 12(4): 359–360
- Bibliography. John Benjamin Murphy. World Cat Identities
Eponymous terms
- Loyal Davis. JB Murphy Stormy petrel of surgery. G.P. Putnam’s sons. 1938
- Gilbert NC. Vasomotor changes in the coronary arteries and their possible significance. JAMA. 1939; 113(22): 1925-1927
- Lawson RS. Murphy’s Triad. Br Med J. 1971; 1(5745): 401–402.
- Salati SA, al Khadi A. Murphy’s sign of cholecystitis– a brief revisit. Journal of Symptoms and Signs. 2012; 1(2): 53-56
- Berger M, Muensterer O, Harmon CM. Tales from previous times: important eponyms in pediatric surgery. Pediatr Surg Int. 2014 Jan;30(1):1-10
- Cadogan M. Murphy’s sign. Eponym A Day. Instagram
[cite]
Dr Michael Leith, Emergency Doctor at a tertiary hospital in Perth, Western Australia | LinkedIn |
