Legg-Calvé-Perthes disease
Description
Legg-Calvé-Perthes disease (LCPD)
LCPD develops as a result of proximal femoral epiphysis ischaemia of unknown aetiology; aka avascular necrosis (AVN) of the proximal femoral head.
The disease is usually insidious in onset and may occur after an injury to the hip. It is most common in male children aged 4-10 years, unilateral in 90% of cases. In cases which are bilateral, the joints are involved successively, not simultaneously.
History of Legg-Calvé-Perthes disease (LCPD)
1897 – Karel Maydl (1853–1903) first publishes on two cases of arthritis deformans coxae in adolescent patients. He gives a detailed pathological description of an abnormal resection of the femoral head in one subject
Ich war daher nicht wenig überrascht, als ich im Jahre 1895 Erkrankungsfälle der Hüftgelenksgegend zu untersuchen Gelegenheit hatte, die einer coxa vara in vielfacher Beziehung ungemein ähnlich, doch nicht als solche aufgefasst werden konnten, sich auch nach einem therapeutischen operativen Eingriffe nicht als solche erwiesen… Wenn auch die traumatische Arthritis deformans eine allgemein bekannt Erkrankung ist, so ist dieselbe bei adolescenten Leuten eine recht seltene Erscheinung und in ihrem klinischen und anatomischen Aussehen recht wenig bekannt.
F.B., 15jährige Schneiderstochter aus Zeltschan, aufgenommen am 16. Mai 1895, gibt folgendes als Anamnese an:…Vor einem Jahre rutschte der Kranken beim Stiegenabwärtsgehen das rechte Bein aus, die Kranke glitt auf der rechten Seite liegend etwa 6 Stufen abwärts…
Der Kopf auffallend plattgedrückt, verbreitert und auch vertical verlängert; seine Projection senkrecht auf die Fläche, birnförmig, mit Verschmälerung nach oben.
I was not unsurprised in the year 1895, when I had the opportunity to examine some cases of diseases of the hip, which were similar in many aspects to coxa vara, though they could not be classified as such, and which proved themselves to be distinct following surgical intervention… Though traumatic arthritis deformans may be a generally well recognized process, its presence in adolescent people is quite rare, and not well known in its clinical and anatomical presentation.
F.B., 15 year old daughter of a tailor from Zeltschan, admitted on 16th May 1895, gives the following history:… A year ago the patient’s right leg slipped from under her whilst descending a staircase, the patient slid down about 6 steps on her right side…
The (femoral) head noticeably squashed, widened and vertically lengthened; in the coronal plane, pearshaped with tapering superiorly.
1909 – Henning Waldenström described a condition of the hip-joint in 10 children under the age of 9 years which he called ‘the upper tuberculous focus in the collum‘. He provided a more detailed report of the disease in his dissertation ‘Die Tuberkulose des collum femoris im Kindersalte ihre Beziehungen zur Huftgelenkentzundung‘, expanded the number of cases to 12 and maintained a tuberculous cause.
1. Fall: Knabe Erich, 14 Jahre alt. Im Alter von 8 Jahren begann der Patient zu hinken, zeitweise konnte er sich nicht auf das rechte Bein stützen… der Arzt der Schule rügte ihn wiederholt, daß er unordentlich wäre, und doch ordentlich zu gehen versuchen sollte…
weiter stellte sich bei der Untersuchung heraus, daß er hinkte, passive Bewegungen waren frei außer Abduktion un Auswärtsrotation; Trochanter aufwärts geschoben. Also das klinische Bild einer Coxa vara…
Röntgenuntersuchung (Fig 1.)…Das Collum bildet mit dem Femurschaft einen Winkel, der kleiner als normal ist. Diese Varusstellung ist… unten durch eine Krümmung des Collum bedingt, oben aber durch eine Zerstörung der oberen Kante des Collum, das dadurch eine mehr horizontale Richtung bekommen hat. Hier liegt also nicht nur eine einfache Krümmung… eine Destruktion ist auch dagewesen…
Das Caput ist in seiner Gesamtheit abgeplattet, nach oben vorgeschoben und hinaus auf den oberen Teil des Collum… so daß ein Teil der oberen Partie des Caput außerhalb der Pfanne liegt und sogar eine Eindrückung von dem oberen Rande der Pfanne erhalten kann
First case: Young boy Erich, 14 years old. At the age of 8 the patient began to limp, at times he couldn’t lean on his right leg… the school doctor reprimands him repeatedly, that he is improper, and that he should try to walk properly…
Examination revealed that he limps, passive movements are unrestricted, except abduction and internal rotation; the trochanter is pushed upwards. So the clinical picture of a Coxa Vara…
X-ray examination (Fig 1.)… The femoral neck forms an angle with the shaft, which is smaller than usual. This varus position is… caused below by a deformity of the neck, above however, by a destruction of the upper edge of the neck, which has thereby acquired a more horizontal orientation. This is therefore not just a simple deformity… a destruction has also taken place…
The femoral head is flattened in its entirety, displaced upwards and outwards on the upper part of the neck… such that the upper part of the head lies partially outside the acetabulum, and even receives an impression from the superior border of the latter.
Above a fantastic and very detailed description by Waldenström of the clinical picture. Unfortunately for him, he postulated (inaccurately) that the aetiology must be infective in nature, tuberculous to be precise. In his paper he makes mention to “foci” innumerable times, which is in reference to the “focal infection theory”- a belief held by many clinicians at the turn of the 20th century, that localized foci of infection were the aetiological cause of many chronic and systemic diseases.
…ein 10jähriger Knabe mit denselben Symptomen und gleichen Konturen auf dem Röntgenbilde wie bei dem eben beschriebenen Fall. Dieser main Fall (Nr.2) hätte also auch unter essentielle Coxa Vara gerechnet werden sollen, wenn nicht die Röntgenaufnahme (Fig 2) mir einen großen Herd- mit allen Zeichen für tuberkulösen Charakter- im oberen Teile des Collum am Caput gezeigt hätte. Der Herd schien einige Sequester zu enthalten, was…dafür sprach, daß er primär war und also die Veränderungen im Caput wahrscheinlich sekundär von Tuberkulose im Collum.
… a 10 year old lad with the same symptoms, and identical contours on x-rays, as in the previously described case. This, my second case, could also have been classified as essential coxa vara, had the X-ray not shown me a large focus- with all signs of Tuberculous character- in the upper part of the femoral head (Fig 2). The focus appears to contain several sequestrations which…speaks for it being primary in aetiology, and thus that the changes in the femoral head are secondary to Tuberculosis in the neck.

1910 – independent of one another, three authors reported a hip disease in children with a symptomatic picture resembling that described by Waldenström. They believed the process as being unrelated to tuberculosis:
Arthur Thornton Legg: 5 cases between the ages of 5 and 8 years. Legg was most inclined to believe that the disease was caused by trauma because he had found such in all of his cases.
“The fifth case (Dr. Goldwaith’s) was a boy of six, who came to him in December, 1908. One year previous he had a fall in which the legs were spread apart. He was lame for a week, and apparently recovered. Seven months later a limp on the left was noticed. He was restless at night and had indefinite pain referred chiefly to the left groin…
The Roentgenogram showed a flattened head and a distinct necrotic area just outside the epiphyseal line in the neck, with apparently some thickening of the neck…
…and at this time it seems to me that a possible explanation of the condition is that the injury may indirectly cause this condition by causing injury or displacement at the epiphyseal line, whereby the nutrition of the head, coming mostly through the neck, is impaired, and by the poorly nourished epiphysis bearing on the acetabulum, it becomes flattened. “
Legg A. 1910

Jacques Calvé: Studied 500 radiographs of children being treated for tuberculosis of the hip joint and found 10 cases of non-tuberculous flattening and fragmentation of the femoral capital epiphysis. Common symptoms: hip pain, limping, restricted movement in the hip-joint especially in regard to abduction, and a palpable enlargement of the caput femoris. Calvé suggested that rickets could be the cause of this newly discovered condition.
En résumé, tous ces cas se ramènent à une arthrite transitoire, de durée courte, se développant sur des sujets porteurs de déformations de l’extrémité supérieure du fémur: coxa vara, hypertrophie de la tête fémorale, atrophie lamellaire du noyeau osseux de l’épiphyse, avec conservation des rapports normaux de surfaces articulaires. Comment faut-il interpréter des lésions osseuses?
Il est naturel, dès qu’il s’agit d’une arthrite chronique de la hanche, de songer à une coxo-tuberculose… A notre avis , ce diagnostic nous parait erroné et nous le rejetons pour plusieurs raisons…
Nous nous trouvons, en effet, en présence d’une ostéogenèse anormale et retardée, ce qui parait plutôt être du ressort du rachitisme. Sans avoir la présomption de conclure, nous avouerons que, jusqu’à plus ample informé, cette solution nous semble la plus plausible.
In summary, all the cases point to a transitory arthritis, of short duration, which develops in those who carry a deformity of the upper extremity of the femur: coxa vara, hypertrophy of the femoral head, atrophy of the lamellar bony nucleus of the epiphysis, with conservation of the normal relations of the articular surfaces. How must one interpret these bony lesions?
It is natural, as soon as one speaks of a chronic arthritis of the hip, to think of a coxo-tuberculosis… In our opinion, this diagnosis seems erroneous, and we reject it for several reasons…
For we are presented with an abnormal and retarded osteogenesis, which appears rather to be the consequence of rickets. Without making the presumption to conclude, we must admit that until we are more informed, this solution seems to us the most plausible.

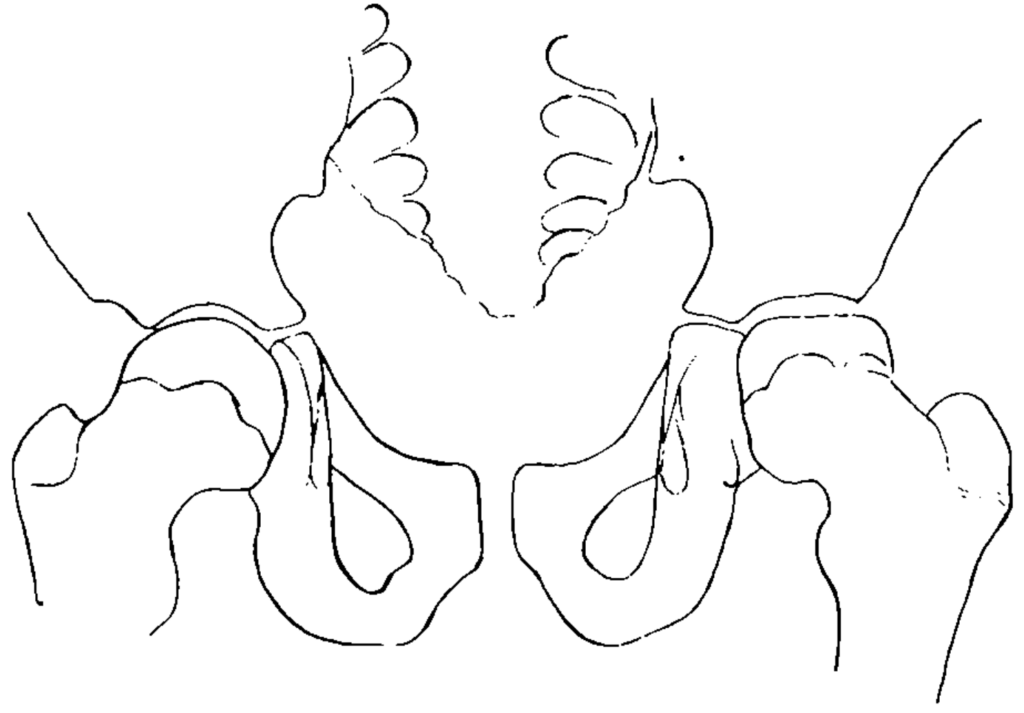
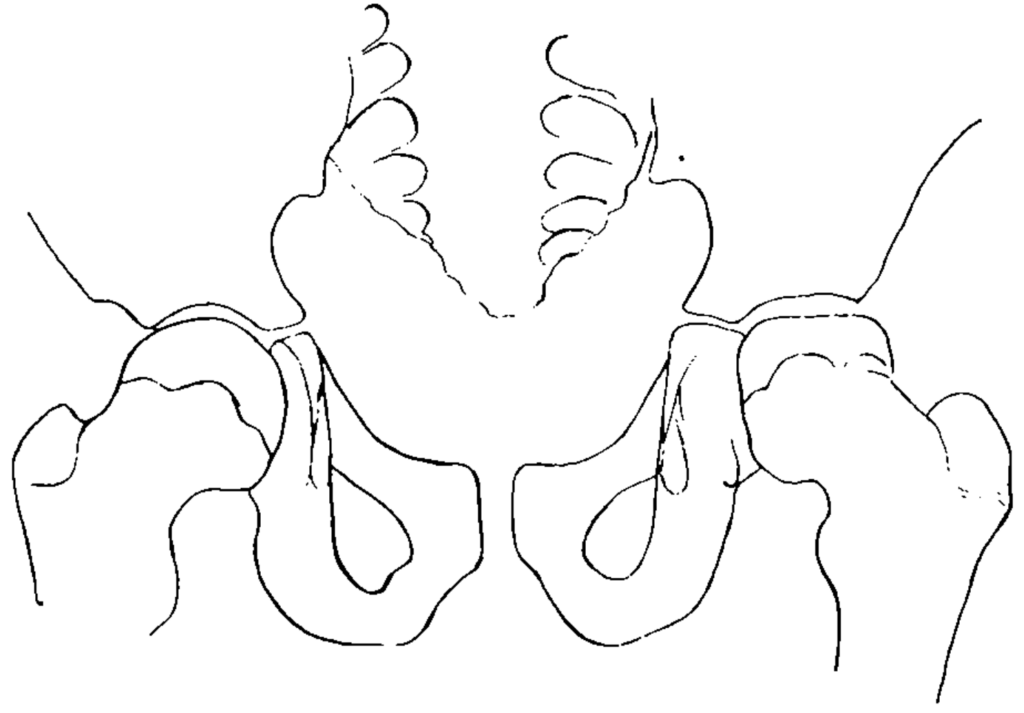
Georg Clemens Perthes: 6 cases, one of which was bilateral. Perthes refuted the importance of trauma but opined the disease he termed ‘Arthritis deformans juvenilis‘ was the result of an inflammatory process in the joint that had occurred during the years of infancy. Furthermore, he commented on the likely importance of poor vasculature being a contributing aetiological factor.
Im Februar 1909 wurde ein 11jähriger Knabe zur Poliklinik gebracht, weil seinen Eltern ein wenig hinkender Gang aufgefallen war. Der Trochanter stand 1 cm über der Roser-Nélatonschen Linie. Schmerzen bestanden weder bei den Beugebewegungen, noch bei Druck auf das Gelenk. Das Röntgenbild zeigte, daß unser erster Gedanke an eine Coxa vara nicht richtig war. Der Schenkelhalswinkel war völlig normal; dagegen zeigte der Schenkelkopf an Stelle der Kugelform die Form eines Kegels…
Wenn wir zum Schluß auf die Ätiologie der juvenilen Arthritis deformans des Hüftgelenks und auf die Auffassung eingehen, welche das Leiden erfahren hat, so stoßen wir nun auf Hypothesen und können nichts anderes tun, als unbewiesene Anschauungen auf ihren Wert prüfen.
Jedenfalls werden wir an der interessanten Möglichkeit nicht zweifeln können, daß die Arthritis deformans juvenilis auf eine anscheinend zunächst ohne Folgen ausgeheilte Hüftgelenksentzündung im Säuglingsalter zurückgeht…
Als ätiologisch bedeutungsvollsten pathologischen Befund betrachtet Wollenberg die von ihm nachgewiesenen Veränderungen kleiner Knochengefäße (Endarteritis obliterans) und Stauungen in den Venen. Diese Veränderungen, die selbst durch verschiedenartige Ursachen hervorgerufen werden, können doch…das Bild der Arthritis deformans hervorrufen, indem der Arterienverschluß zu Ernährungsstörungen im Knochen, die Stauung zu Wucherungsvorgängen führt.
In February 1909 an 11 year old lad was brought to the clinic, as his parents had noticed a somewhat limping gait. The trochanter lay 1cm above the Roser-Nélaton line. Pain was not elicited on active movement, nor with pressure on the joint. The X-ray showed that our initial thought of Coxa vara was not correct. The femoral neck was completely normal; in contrast the femoral head appeared to have a conical, rather than a rounded shape.
To end, if we consider the aetiology of the juvenile Arthritis deformans, and the conception of this illness, we encounter hypotheses and can do nothing other than test unproven opinions for their merit.
In any case we cannot doubt of the interesting possibility, that the juvenile arthritis deformans can be traced back to a seemingly initially inconsequential inflammation of the hip in infancy.
The most aetiologically significant pathological discovery, according to Wollenberg, it the changes he has demonstrated in the small bony vasculature (Endarteritis obliterans), and the venous congestion. These changes, which can be the sequel of different causes themselves, can indeed…create the picture of arthritis deformans, whereby the arterial closure can lead to nutritional deficiencies in the bone, and the congestion to proliferative processes.
Classification
The classifications for LCPD can be divided into the one that defines the stage of the disease and the ones used to prognosticate outcome.
1922 – Waldenström classification defines 4 radiographic stages of LCPD during the active phase of the disease, termed the initial stage, fragmentation stage, re-ossification stage, and residual stage, according to characteristic radiographic features.
1971 – Catterall classification: four-stage classification based on the radiographic appearance of the femoral epiphysis
1992 – Herring defined the Lateral pillar classification and is the most widely used for predicting the final outcome at the onset of fragmentation. Developed on data from 86 patients (93 hips) treated non-operatively and based on the appearance of the lateral pillar of the proximal femoral epiphysis on the AP X-ray at the onset of fragmentation. Divided into three groups: A, normal lateral pillar; B, lateral pillar >50% of its original height; and C, lateral pillar ≤ 50% of its original height.
2004 – Herring et al provided the first rigorously conducted evaluation of non-operative and surgical treatments of LCPD. A prospective multicentre design was used to study the outcomes of 345 hips from symptom onset to skeletal maturity. Outcomes were analysed according to age at symptom onset, modified lateral pillar group(A, B, B/C, or C) and treatment. The available evidence indicates that non-operative treatment alone fails to improve the long-term outcome. Surgery improves the outcomes of patients with extensive epiphyseal involvement and older age at onset.
Associated Persons
- Karel Maydl (1853–1903)
- Arthur Thornton Legg (1874–1939)
- Jacques Calvé (1875–1954)
- Georg Clemens Perthes (1869–1927)
- Johann Henning Waldenström (1877–1972)
Alternative names
- Perthes disease
- Legg–Perthes disease
- Calve-Legg-Perthes-Waldenström disease
- Coxa plana
References
Historical references
- Maydl K. Coxa vara und Arthritis deformans coxae. Wiener klinische Rundschau 1897; 11: 153-154.
- Waldenström H. Der obere tuberkulöse Cullumherd. Zeitschrift für Orthopädische Chirurgie 1909; 24: 487–512.
- Waldenström H. Die Tuberkulose des collum femoris im Kindersalte ihre Beziehungen zur Huftgelenkentzundung, Stockholm. 1910
- Legg AT. An obscure affection of the hip-joint. The Boston medical and surgical journal 1910; 162: 202–204. [Reprint: Clin Orthop Relat Res. 2006 Oct;451:11-3. PMID 17038923]
- Calvé J. Sur une forme particulière de pseudo-coxalgie greffée sur des déformations caractéristiques de l’extrémité supérieure du fémur. Revue de chirurgie 1910; 42: 54–84
- Perthes G. Über Arthritis deformans juvenilis. Deutsche Zeitschrift für Chirurgie. 1910; 107: 111–159. [Perthes G.On juvenile arthritis deformans. 1910. Clin Orthop Relat Res. 2012; 470(9): 2349-2368]
- Waldenström H. The Definite Form of the Coxa Plana. Acta Radiologica, 1922; 1(4): 384-394
- Waldenström H. On coxa plana. Osteochondritis deformans coxae juvenilis. Leggs disease, maladie de Calvé, Perthes krankheit. Acta chirurgica Scandinavica. 1923; 55: 577–590.
- Waldenström H. The First Stages of Coxa Plana. Acta Orthopaedica Scandinavica. 1934;5:1-4, 1-34
Modern interpretation
- Jonsäter S. A Histo-Pathologic and Arthrografic Study. Acta Orthopaedica Scandinavica. 1953;24:sup12, 1-98
- Catterall A. The natural history of Perthes’ disease. J Bone Joint Surg Br. 1971; 53(1): 37-53
- Stulberg SD, Cooperman DR, Wallensten R. The natural history of Legg-Calvé-Perthes disease. J Bone Joint Surg Am. 1981 Sep;63(7):1095-108.
- Herring JA, Neustadt JB, Williams JJ, Early JS, Browne RH. The lateral pillar classification of Legg-Calvé-Perthes disease. J Pediatr Orthop. 1992; 12(2): 143-150
- Herring JA, Kim HT, Browne R. Legg-Calve-Perthes disease. Part I: Classification of radiographs with use of the modified lateral pillar and Stulberg classifications. J Bone Joint Surg Am. 2004; 86(10): 2103-20
- Herring JA, Kim HT, Browne R. Legg-Calve-Perthes disease. Part II: Prospective multicenter study of the effect of treatment on outcome. J Bone Joint Surg Am. 2004; 86(10): 2121-34.
- Fornari ED, Karkenny A, Schulz J. Legg-Calvé-Perthes disease. Current Orthopaedic Practice. 2015;26(5):487-493.
- Wenger DR, Pandya NK. A brief history of Legg-Calvé-Perthes disease. J Pediatr Orthop. 2011 Sep;31(2 Suppl):S130-6.
- Rampal V, Clément JL, Solla F. Legg-Calvé-Perthes disease: classifications and prognostic factors. Clin Cases Miner Bone Metab. 2017; 14(1): 74–82
- Leroux J, Abu Amara S, Lechevallier J. Legg-Calvé-Perthes disease. Orthop Traumatol Surg Res. 2018; 104(1S): S107-S112
[cite]
eponymictionary
the names behind the name
