Neuro 101: Cerebral Hemispheres
Frontal Lobe
Clinicoanatomic correlation
- Motor function
- Controlled by motor cortex
- Corticospinal tract
- origin of the primary motor tract from the brain to the spinal cord
- Left side of brain controls right side of body and vice versa
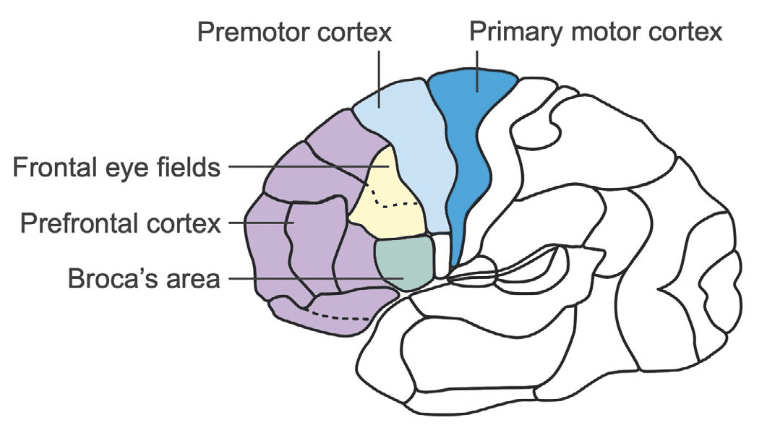
Executive Functions
- Controlled by the prefrontal cortex
- Involve:
- Focus and concentration
- Regulation of motor and sensory input
- Planning and initiating actions
- Maintaining task performance
- Self-monitoring and correction
Learned Motor Patterns
- Controlled by the premotor cortex
- Examples include habitual or rehearsed actions such as climbing stairs
Volitional Eye Movements
- Controlled by the frontal eye fields
- Key directional behaviours:
- Activation of the right frontal eye field turns the eyes to the left
- Stroke: eyes deviate toward the lesion
- Seizure: eyes deviate away from the lesion
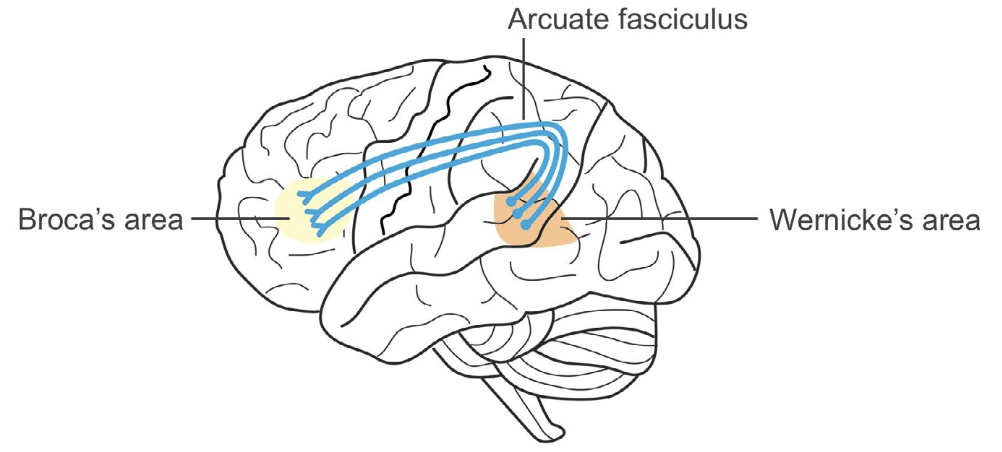
Speech and Language
- Broca’s area (in the frontal lobe) coordinates speech production
- It works in conjunction with Wernicke’s area (in the temporal lobe) for language comprehension
Broca’s Aphasia
- Results from damage to the dominant hemisphere
- In right-handed individuals and most left-handed individuals, this is the left hemisphere
- Features include:
- Halting or hesitant speech
- Word substitutions
- Omission of small linking words (e.g., articles and prepositions)
- Impaired repetition of phrases
Temporal Lobe
Important regions
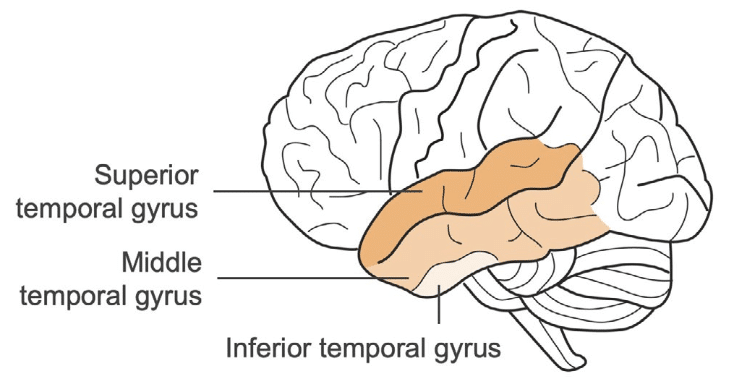
Clinicoanatomic Correlation
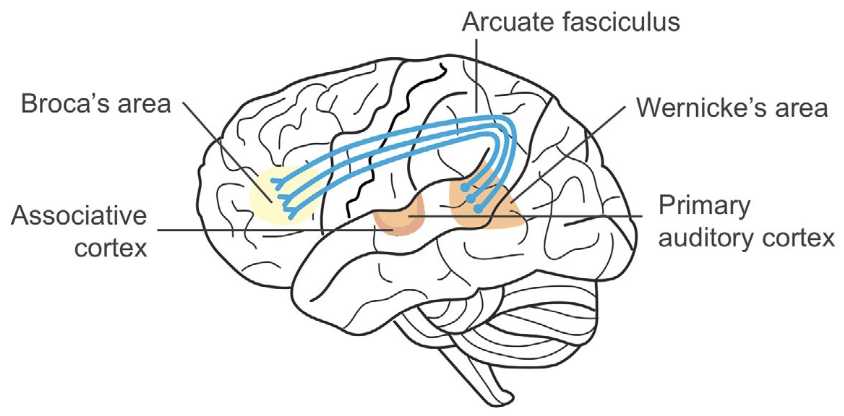
Hearing
- Primary auditory cortex: responsible for hearing and initial sound processing
- Associative auditory cortex: interprets spoken and written language
- Cortical deafness: requires bilateral temporal lobe lesions (extremely rare)
Language
- Wernicke’s area: essential for language comprehension
- Wernicke’s aphasia:
- Occurs with damage to the dominant hemisphere
- Produces fluent but meaningless speech
- Marked difficulty understanding spoken language
- Wernicke’s aphasia:
- Associative aphasia (conduction aphasia):
- Results from damage to the arcuate fasciculus
- Characterised by:
- Inability to repeat spoken language
- Difficulty writing coherent language
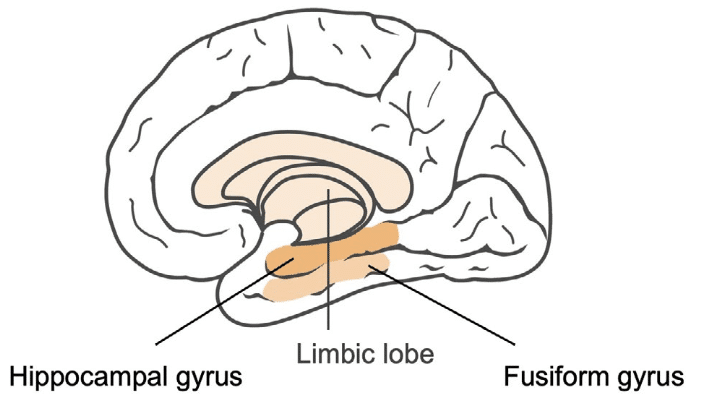
Emotions and Memory
- Governed by the limbic lobe
- Bilateral lesions of the hippocampus and thalamus can result in profound memory loss
Temporal Lobe Seizures
- Often begin in the first or second decade of life
- Common features:
- Visual or auditory hallucinations
- Olfactory hallucinations
- Automatisms (e.g. lip-smacking, repetitive movements)
- Déjà vu or jamais vu
- Clouding of consciousness
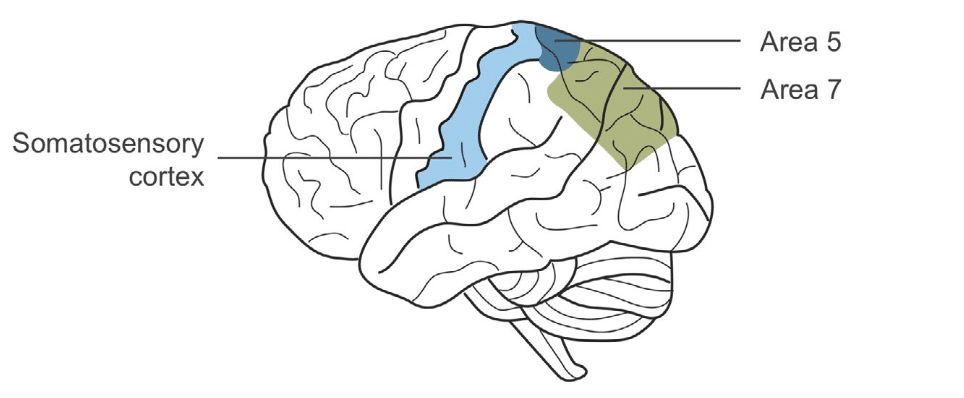
Parietal Lobe
Clinicoanatomic Correlation
Sensory Function
- Mediated by the primary somatosensory cortex and associative cortices (Brodmann areas 5 and 7)
- Cutaneous sensibility:
- Pinprick
- Temperature
- Light touch
- Vibration
- Proprioception
- Cortical sensibility:
- Two-point discrimination
- Graphesthesia
- Stereognosis
- Double simultaneous stimulation
- Somatognosia
Extinction
- Inability to perceive multiple simultaneous stimuli of the same type (e.g., tactile or visual)
- Typically occurs in the contralesional field
Neglect
- Failure to perceive or attend to stimuli on one side of the body
- Often occurs with non-dominant hemisphere lesions (usually right-sided)
Parietal Stroke Symptoms
General Signs
- Agraphesthesia
- Loss of two-point discrimination
- Astereognosis
- Extinction
Dominant Hemisphere Involvement
- Right-left confusion
- Finger agnosia
- Acalculia
- Agraphia
These features together comprise Gerstmann syndrome
Other Symptoms
- Asomatognosia (unawareness of parts of one’s own body)
- Dressing apraxia
- Constructional apraxia
- Geographic disorientation
Occipital Lobe
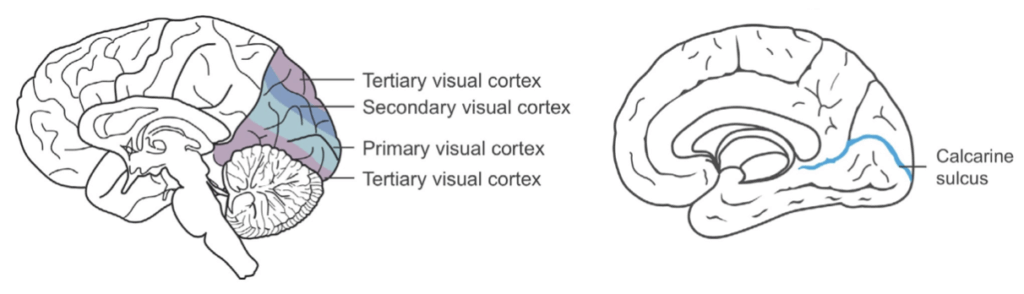
Clinicoanatomic Correlation
Calcarine Cortex
- Located within the calcarine fissure
- Critical for visual processing
Cortical Blindness
- Requires bilateral occipital lobe lesions
- May result in Anton’s syndrome:
- Patient is unaware of blindness
- May confabulate visual experiences
Disconnection Syndrome
- Occurs due to lesion in left (dominant) visual cortex and corpus callosum
- Causes loss of input from the right visual field
- Corpus callosum damage prevents information transfer to left parietal language areas
- Produces alexia without agraphia:
- Patient cannot read (alexia)
- But can still write (agraphia not affected)
Integrated Concepts
Sensory and Motor Homunculi
- The homunculus is a visual representation mapping body parts to their corresponding motor and sensory cortical areas
- Areas requiring fine control or sensation (e.g. hands, face) occupy larger cortical regions
Visual Field Deficits
- Can occur due to damage anywhere along the visual pathway: retina, optic nerves, chiasm, tracts, radiations, or occipital cortex
- Lesions in the occipital lobe commonly cause homonymous hemianopia
Blood Supply of the Brain
Anterior Circulation
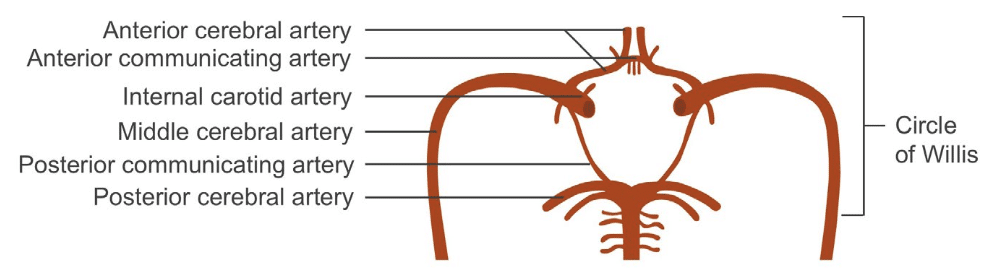
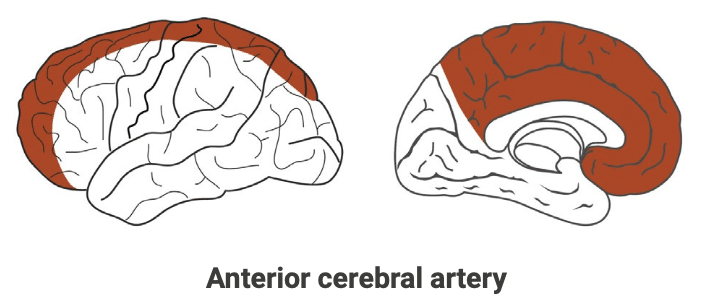
Anterior Cerebral Artery (ACA) Stroke
- Contralateral sensory-motor deficits, especially affecting leg and foot
- Eyes and head often deviate towards the lesion
- Rigidity may be present
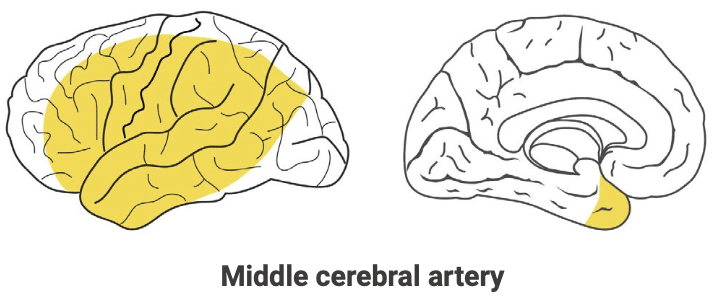
Middle Cerebral Artery (MCA) Stroke
- Contralateral hemiplegia, more pronounced in face, arm and shoulder
- Hemianaesthesia (sensory loss)
- Homonymous hemianopia
- Eyes deviate towards the lesion
- Dominant hemisphere involvement:
- Aphasia (Broca’s, Wernicke’s or global)
- Non-dominant hemisphere involvement:
- Agnosia
- Neglect
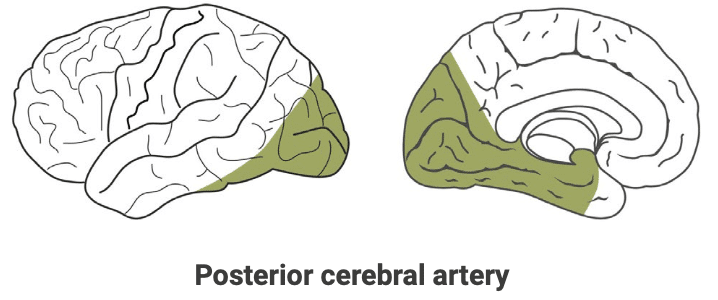
Posterior Cerebral Artery (PCA) Stroke
- Involves occipital lobe, particularly the calcarine cortex and optic radiations
- Causes homonymous hemianopia
Posterior Circulation Stroke
- Typically produces bilateral or crossed symptoms
- Clinical features:
- Headache
- Nausea and vomiting
- Vertigo
- Nystagmus
- Limb weakness
- Extraocular movement abnormalities
- Ataxia
The “D” Symptoms of Posterior Stroke
- Dizziness
- Dysarthria
- Disequilibrium (or dysataxia)
- Deafness
- Diplopia
- Dysphagia
- Dysphonia
This is an edited excerpt from the Medmastery course Clinical Neurology Essentials by Robert Coni, DO, EdS, FAAN. Acknowledgement and attribution to Medmastery for providing course transcripts.
- Coni R. Headache Masterclass. Medmastery
- Simmonds GR. Neurology Masterclass: Managing Common Diseases. Medmastery
- Simmonds GR. Neurology Masterclass: Managing Emergencies. Medmastery
Clinical Neurology Essentials
- Coni R. Neuro 101: Neurological Examination. LITFL
- Coni R. Neuro 101: Cerebral Hemispheres. LITFL
- Coni R. Neuro 101: Cerebellum and Basal Ganglia. LITFL
- Coni R. Neuro 101: Brainstem. LITFL
- Coni R. Neuro 101: Cranial Nerves. LITFL
- Coni R. Neuro 101: Spinal Cord. LITFL
- Coni R. Neuro 101: Peripheral Nervous System. LITFL
References
Further reading
- Brazis PW, Masdeu JC, Biller J. Localization in Clinical Neurology. 8e 2021
- Campbell WW. DeJong’s The Neurologic Examination. 8e 2019
- Fuller G. Neurological Examination Made Easy. 6e 2019
- Kiernan J. Barr’s The Human Nervous System: An Anatomical Viewpoint. 10e 2015
- O’Brien M. Aids to the Examination of the Peripheral Nervous System. 6e 2023
- Patten JP. Neurological Differential Diagnosis. 2e 1996
- Waxman SG. Correlative Neuroanatomy. 23e 1996
Publications
- Carrera E, Michel P, Bogousslavsky J. Anteromedian, central, and posterolateral infarcts of the thalamus: three variant types. Stroke. 2004 Dec;35(12):2826-31.
- Datar S, Rabinstein AA. Cerebellar infarction. Neurol Clin. 2014 Nov;32(4):979-91
- Fama ME, Turkeltaub PE. Treatment of poststroke aphasia: current practice and new directions. Semin Neurol. 2014 Nov;34(5):504-13
- Fanciulli A, Wenning GK. Multiple-system atrophy. N Engl J Med. 2015 Jan 15;372(3):249-63.
- Kelly PJ, Stein J, Shafqat S, Eskey C, Doherty D, Chang Y, Kurina A, Furie KL. Functional recovery after rehabilitation for cerebellar stroke. Stroke. 2001 Feb;32(2):530-4.
- Kwong Yew K, Abdul Halim S, Liza-Sharmini AT, Tharakan J. Recurrent bilateral occipital infarct with cortical blindness and anton syndrome. Case Rep Ophthalmol Med. 2014;2014:795837.
- Li K, Malhotra PA. Spatial neglect. Pract Neurol. 2015 Oct;15(5):333-9. doi: 10.1136/practneurol-2015-001115. Epub 2015
Neurology Library
Robert Coni, DO, EdS, FAAN. Vascular neurologist and neurohospitalist and Neurology Subspecialty Coordinator at the Grand Strand Medical Center in South Carolina. Former neuroscience curriculum coordinator at St. Luke’s / Temple Medical School and fellow of the American Academy of Neurology. In my spare time, I like to play guitar and go fly fishing. | Medmastery | Linkedin |

