Neuro 101: Spinal Cord
In this section, we will cover the anatomical structure of the spinal cord and vertebral column, spinal nerve organisation, blood supply, motor and sensory pathways, clinical examination principles, myotomes and dermatomes, localisation of spinal cord lesions, and common spinal cord syndromes.
Function
The spinal column encases and protects the spinal cord, which serves as a conduit for motor, sensory, and autonomic signals between the brain and the body.
- Conducts ascending sensory information from the periphery to the brain
- Conducts descending motor commands from the brain to the periphery
- Mediates reflex activity independently of the brain
Testing
Clinical examination of spinal cord function involves assessing motor, sensory, and autonomic pathways.
- Identify segmental level by examining myotomes and dermatomes
- Assess for patterns of weakness or sensory loss that respect spinal levels
- Evaluate reflexes for hyperreflexia (upper motor neuron signs) or hyporeflexia (lower motor neuron signs)
- Observe for bladder, bowel, and sexual dysfunction in suspected cord lesions
- Neuroimaging (MRI) is the investigation of choice for suspected spinal cord pathology
Pathology
Anatomy
- Vertebrae:
- 7 cervical
- 12 thoracic
- 5 lumbar
- 5 sacral
- Spinal nerves:
- 8 cervical
- 12 thoracic
- 5 lumbar
- 5 sacral
- The spinal cord terminates at the L2 vertebral body (conus medullaris). Nerve roots below this level travel as the cauda equina.
Discrepancy exists between spinal segments and vertebral levels:
- C1–C4 → C1–C4 vertebrae
- C5–C8, T1–T4 → C4–T3 vertebrae
- T5–T8 → T3–T6 vertebrae
- T9–T12 → T6–T9 vertebrae
- L1–L5 → T10–T12 vertebrae
- S1–S5, Co1 → L1 vertebra
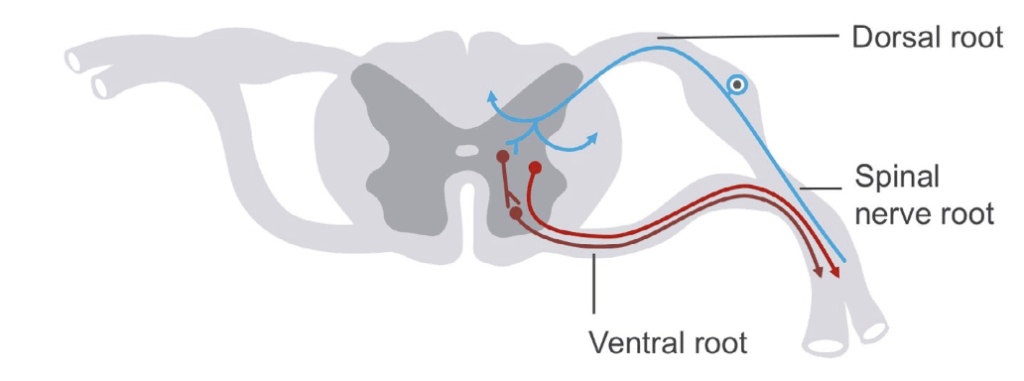
Afferent (or sensory) input to the nervous system arrives in the spinal cord via the dorsal root.
Efferents (or motor output) exit via the ventral root.
Grey matter
- Central location within the cord
- Anterior horn: motor neurons
- Lateral horn: autonomic neurons
- Posterior horn: sensory interneurons
White matter tracts
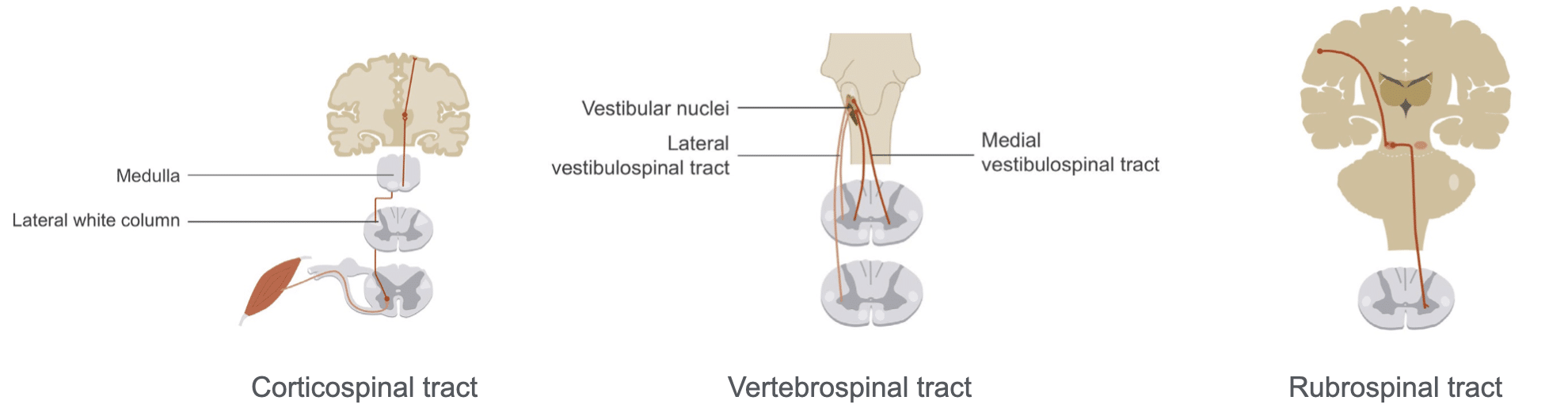
Descending tracts:
- Corticospinal tract:
- motor control; crosses in medulla (pyramidal decussation); Left brain controls right body and right brain controls left body
- Vestibulospinal tracts:
- Carry information from vestibular nuclei in brainstem to spinal cord
- Important for rapid correction of neck movement and posture (in response to changing body position)
- Rubrospinal tract:
- Carries information from red nucleus to anterior horn cells
- Modulates voluntary motor movements
- Fibers cross before descending in lateral columns
Ascending tracts:
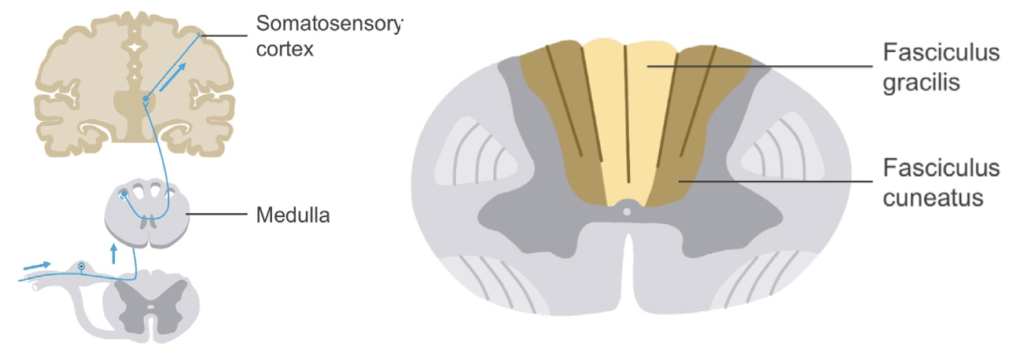
- Posterior columns:
- Proprioception, vibration, fine touch, two-point discrimination
- Fibers cross at spinal cord then ascend
- Somatotopic organization: fasciculus gracilis and cuneatus
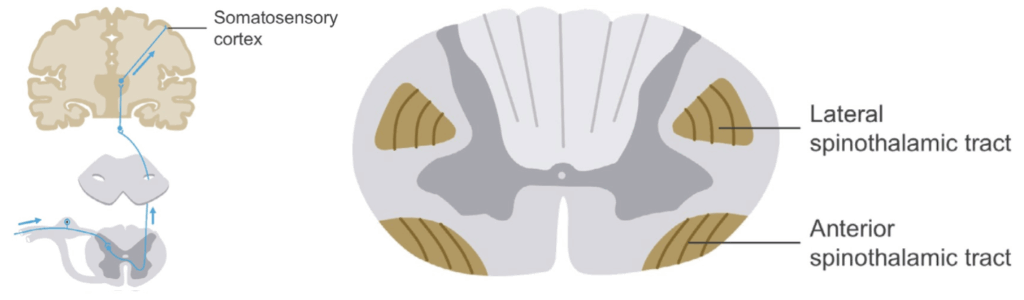
- Spinothalamic tract:
- Carries sensory information from periphery to cortex
- pain and temperature (lateral spinothalamic tract)
- light touch (anterior spinothalamic tract)
- Somatotopic organization
- Carries sensory information from periphery to cortex
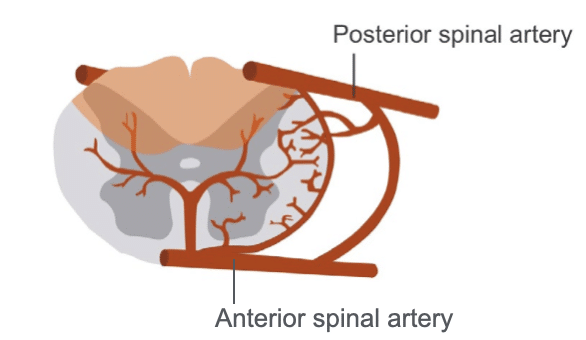
Blood supply
- Anterior spinal artery: anterior two-thirds of cord
- Posterior spinal arteries: posterior third of cord
- Radicular arteries: reinforcements from the thoracic aorta and the abdominal aorta, which supply the ventral and dorsal roots as well as the cord.
- largest radicular artery is the spinal artery of Adamkiewicz; important in the thoracic and lumbar regions; can be damaged during surgery on the aorta.
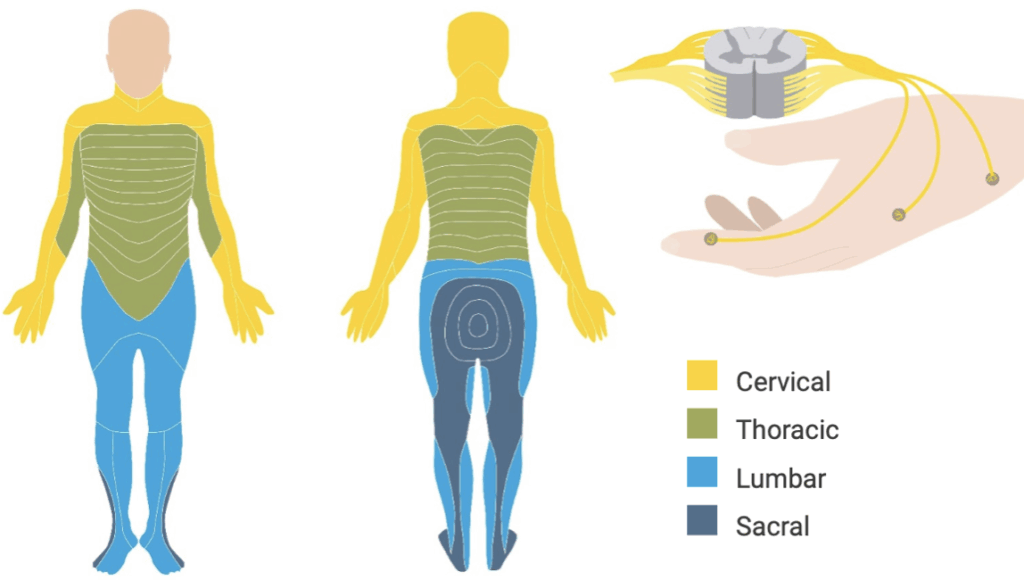
Myotomes
A myotome refers to all the muscles or groups of muscles innervated by the motor horn cells within a segment of the cord.
- Upper limb:
- C5: shoulder control
- C6: elbow flexion/extension
- C7: wrist movement
- C8: finger flexion/extension
- T1: intrinsic hand muscles
- Lower limb:
- L1–L2: hip flexion
- L3–L4: knee extension
- L5–S2: knee flexion
- L4: ankle dorsiflexion
- L5: great toe extension
- S1–S2: plantarflexion
- S2–S3: toe adduction
Dermatomes
- A dermatome is a region of skin or a structure, which has somatic afferent sensory innervation provided by a single spinal cord segment and a single nerve root.
Localising spinal cord lesions
- Exclude cranial nerve involvement to confirm spinal origin
- Define level by identifying sensory or motor loss pattern
- Crossed signs suggest brainstem lesion
- Same-sided head and body signs suggest cerebral lesion
During and after your examination you should seek answers to the following questions.
- Which tracts are involved?
- Which side is involved?
- What level is involved?
- Are upper motor neurons or lower motor neurons involved?
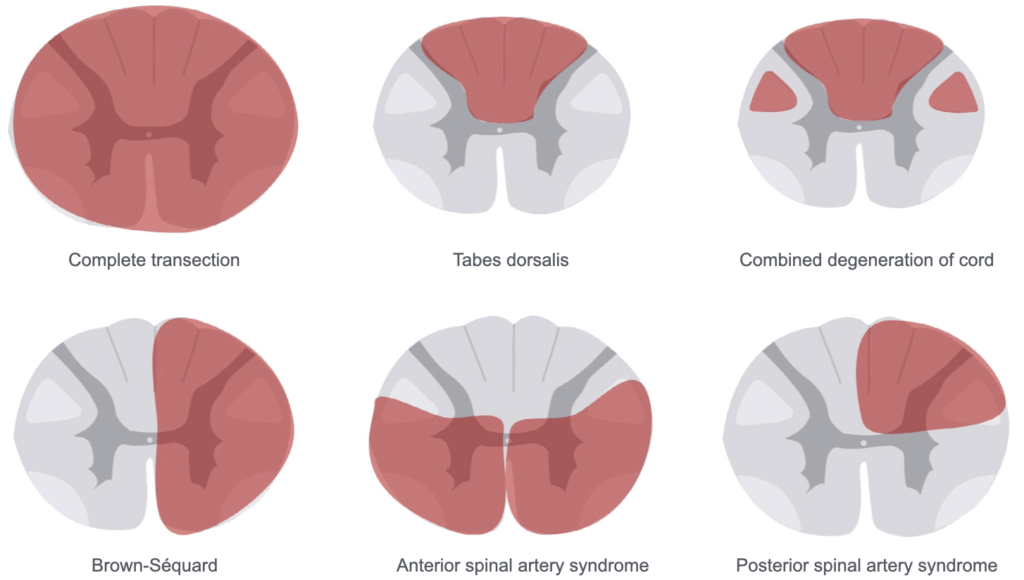
Spinal cord syndromes
Small central lesion:
- Affects crossing spinothalamic tract fibers
- Bilateral loss of pain and temperature
- Proprioception and vibration preserved
- Causes: syrinx, expanded central canal
Large central cord lesion:
- Bilateral pain/temperature loss
- Lower motor neuron signs at level, upper motor neuron signs below
- Sacral sparing possible (external compression produces sacral anaesthesia)
- Causes: multiple sclerosis, tumours, astrocytoma
Brown-Séquard syndrome (hemisection):
- Ipsilateral proprioception, vibration loss and and two-point discrimination below lesion
- Ipsilateral loss of pain and temperature sensation at level of lesion
- Contralateral pain/temperature loss 1–2 levels below lesion
- Lower motor neuron signs at level, upper motor neuron signs below
- Causes: penetrating injury, tumour, haemorrhage
Complete transection:
- Bilateral motor and sensory loss below lesion
- Lower motor neuron signs at level, upper motor neuron signs below
- Spinal shock initially; total flaccidity early after injury
- Autonomic dysfunction (bladder, bowel, respiration if above C5)
- Causes: trauma, transverse myelitis, tumour, penetrating injury, haemorrhage
Combined degeneration of the cord:
- Bilateral proprioception and vibration loss
- Bilateral motor loss
- Pain and temperature preserved
- Causes: B12 deficiency, nitrous oxide abuse, copper deficiency
Tabes dorsalis:
- Most often bilateral damage (affecting legs)
- Loss of proprioception, sensory ataxia, lightning pains
- Loss of reflexes, hypotonia
- Cause: tertiary syphilis
Anterior spinal artery syndrome:
- Bilateral pain/temperature loss
- Proprioception and vibration sense remain intact
- Bilateral loss of motor activity below lesion
- Lower motor neuron signs at level, upper motor neuron signs below
- Causes: aortic surgery, hypotension, atherosclerosis, Adamkiewicz injury
Posterior spinal artery syndrome:
- Ipsilateral total sensory loss at level
- Loss of segmental reflexes at level of lesion
- Ipsilateral loss of proprioception and vibration sense below lesion
Clinical Neurology Essentials
- Coni R. Neuro 101: Neurological Examination. LITFL
- Coni R. Neuro 101: Cerebral Hemispheres. LITFL
- Coni R. Neuro 101: Cerebellum and Basal Ganglia. LITFL
- Coni R. Neuro 101: Brainstem. LITFL
- Coni R. Neuro 101: Cranial Nerves. LITFL
- Coni R. Neuro 101: Spinal Cord. LITFL
- Coni R. Neuro 101: Peripheral Nervous System. LITFL
References
Further reading
- Brazis PW, Masdeu JC, Biller J. Localization in Clinical Neurology. 8e 2021
- Campbell WW. DeJong’s The Neurologic Examination. 8e 2019
- Fuller G. Neurological Examination Made Easy. 6e 2019
- Kiernan J. Barr’s The Human Nervous System: An Anatomical Viewpoint. 10e 2015
- O’Brien M. Aids to the Examination of the Peripheral Nervous System. 6e 2023
- Patten JP. Neurological Differential Diagnosis. 2e 1996
- Waxman SG. Correlative Neuroanatomy. 23e 1996
Publications
- Biousse V, Newman NJ. Ischemic Optic Neuropathies. N Engl J Med. 2015 Jun 18;372(25):2428-36.
- Davidovic L, Ilic N. Spinal cord ischemia after aortic surgery. J Cardiovasc Surg (Torino). 2014 Dec;55(6):741-57.
Neurology Library
Robert Coni, DO, EdS, FAAN. Vascular neurologist and neurohospitalist and Neurology Subspecialty Coordinator at the Grand Strand Medical Center in South Carolina. Former neuroscience curriculum coordinator at St. Luke’s / Temple Medical School and fellow of the American Academy of Neurology. In my spare time, I like to play guitar and go fly fishing. | Medmastery | Linkedin |

