Neuro 101: Neurological Examination
The Neurological Examination
The eight steps:
- Mental status examination
- Cranial nerve examination
- Motor examination
- Reflex examination
- Special reflex examination
- Sensory examination
- Cerebellar examination
- Gait and station examination
Mental status examination
Assess:
- Appearance and mood
- Higher cortical functions:
- Speech
- Attention
- Orientation
- Memory
- Calculation
- Perception and praxis
Aphasia refers to a dysfunction of language, either production and/or comprehension.
Dysarthria refers to a dysfunction of the mechanical process of speech production, while language processing remains normal.
Neglect is typically due to a non-dominant hemisphere injury (usually the right side) and leads to neglect of the opposite side of the body. This may involve the visual field, sensory input, or body awareness (asomatognosia). Individuals may extinguish stimuli from the left side when both sides are stimulated simultaneously.
Cranial nerve examination
Group cranial nerve testing by function:
- Smell – CN I
- Eye movements and vision – CN II, III, IV, VI
- Facial movement and sensation – CN V, VII
- Hearing and balance – CN VIII
- Oromandibular function and sensation – CN IX, X, XII
- Sternocleidomastoid and trapezius muscles – CN XI
Motor examination
Differentiate between upper motor neuron (UMN) and lower motor neuron (LMN) lesions.
Upper motor neuron signs:
- Hypertonicity
- Hyperreflexia
- Babinski response (extensor plantar)
- Clonus
Lower motor neuron signs:
- Flaccid tone
- Muscle wasting and atrophy
- Hyporeflexia
- Fasciculations
Test muscle strength using the Medical Research Council (MRC) grading system.
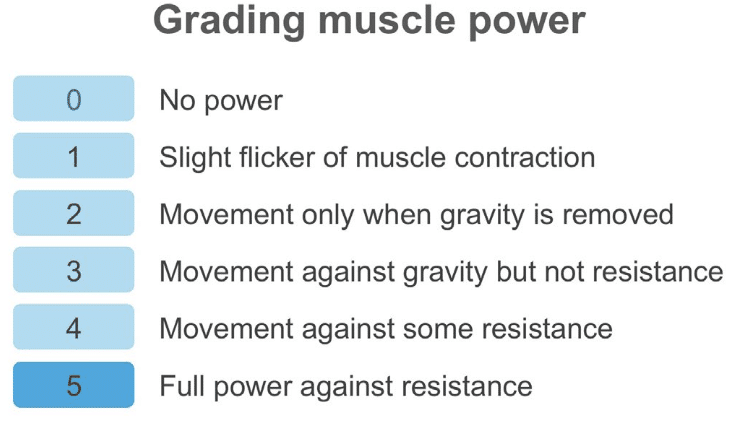
The Medical Research Council grading system remains the standard, but research has shown that there are difficulties with inter-observer reliability. An alternative method with simpler criteria has been proposed.
- 0 = Paralysis
- 1 = Severe weakness
- 2 = Slight weakness
- 3 = Normal strength
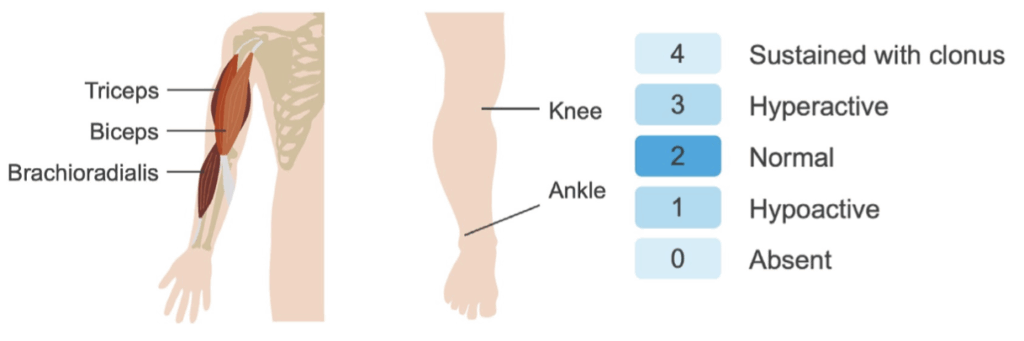
Reflex examination
Reflexes help distinguish UMN from LMN lesions.
- UMN: Brisk reflexes
- LMN: Diminished or absent reflexes
Elicit reflexes by tapping the tendon and observing for muscle contraction.
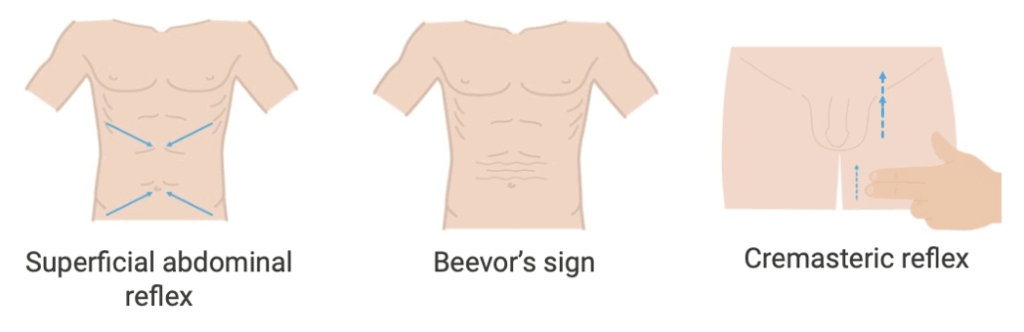
Special reflex examination
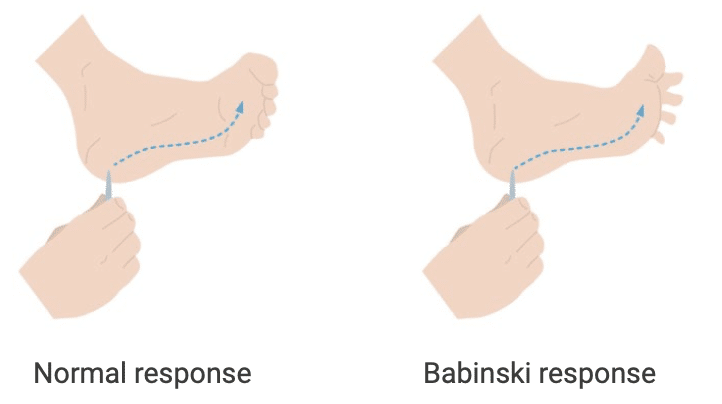
Plantar reflex:
Gently stroke the sole from heel to toe and observe the big toe’s response.
- Downward movement = normal (flexor response)
- Upward movement = abnormal (Babinski/extensor response) → indicates UMN lesion or corticospinal tract involvement.
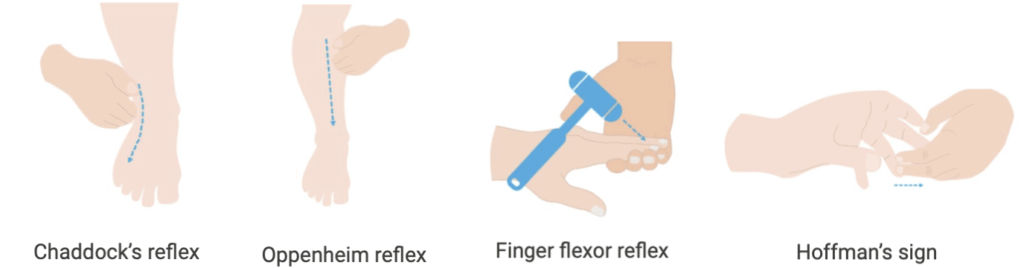
Other reflexes
- Chaddock sign – alternative/complementary test to the Babinski reflex to test the integrity of the corticospinal tract.
- Oppenheim reflex – a pathologic reflex that indicates a loss of cortical inhibition and is associated with upper motor neuron lesions
- Beevor sign – Upward movement of the umbilicus with truncal flexion from a supine position, associated with a spinal cord lesion between the levels of T10 and T12
Sensory examination
Cutaneous sensibilities:
- Pinprick
- Temperature
- Light touch
- Vibration
- Proprioception
Cortical sensibilities:
- Two-point discrimination
- Graphesthesia
- Stereognosis
- Double simultaneous stimulation
Start sensory testing in areas of suspected loss and work towards regions of normal sensation.
Cerebellar examination
Pronator drift:
Push the patient’s arms down gently. A delay in return or bouncing suggests cerebellar dysfunction.
Coordination:
- Observe for ataxia during gait or limb testing.
- Test upper limbs with finger-to-nose-to-finger.
- Test lower limbs with heel-to-shin.
- Tone is generally decreased in cerebellar disease.
Gait and station examination
Gait assessment:
- Symmetry
- Pain
- Stooping
- Circumduction
- Hip hiking
- Steppage
- Speed
- Step width
Common gait patterns:
- Parkinsonian gait: Festinating, hesitant, stop-start motion
- Ataxic gait: Uncoordinated, veering due to sensory or cerebellar dysfunction
- Apraxic gait: Appears as if the patient has forgotten how to walk; seen with frontal lobe lesions or normal pressure hydrocephalus
- Hemiplegic gait: Swinging of one leg, commonly post-stroke
This is an edited excerpt from the Medmastery course Clinical Neurology Essentials by Robert Coni, DO, EdS, FAAN. Acknowledgement and attribution to Medmastery for providing course transcripts.
- Coni R. Headache Masterclass. Medmastery
- Simmonds GR. Neurology Masterclass: Managing Common Diseases. Medmastery
- Simmonds GR. Neurology Masterclass: Managing Emergencies. Medmastery
Clinical Neurology Essentials
- Coni R. Neuro 101: Neurological Examination. LITFL
- Coni R. Neuro 101: Cerebral Hemispheres. LITFL
- Coni R. Neuro 101: Cerebellum and Basal Ganglia. LITFL
- Coni R. Neuro 101: Brainstem. LITFL
- Coni R. Neuro 101: Cranial Nerves. LITFL
- Coni R. Neuro 101: Spinal Cord. LITFL
- Coni R. Neuro 101: Peripheral Nervous System. LITFL
References
Further reading
- Brazis PW, Masdeu JC, Biller J. Localization in Clinical Neurology. 8e 2021
- Campbell WW. DeJong’s The Neurologic Examination. 8e 2019
- Fuller G. Neurological Examination Made Easy. 6e 2019
- Kiernan J. Barr’s The Human Nervous System: An Anatomical Viewpoint. 10e 2015
- O’Brien M. Aids to the Examination of the Peripheral Nervous System. 6e 2023
- Patten JP. Neurological Differential Diagnosis. 2e 1996
- Waxman SG. Correlative Neuroanatomy. 23e 1996
Neurology Library
Robert Coni, DO, EdS, FAAN. Vascular neurologist and neurohospitalist and Neurology Subspecialty Coordinator at the Grand Strand Medical Center in South Carolina. Former neuroscience curriculum coordinator at St. Luke’s / Temple Medical School and fellow of the American Academy of Neurology. In my spare time, I like to play guitar and go fly fishing. | Medmastery | Linkedin |

