Norman Barrett
Norman Rupert Barrett (1903-1979) was an Australian-born British cardiothoracic surgeon.
Educated at Eton, Trinity College Cambridge, and St. Thomas’ Hospital, London, he rose to become one of the foremost figures in thoracic surgery in mid-twentieth-century Britain. His Rockefeller Travelling Fellowship to the Mayo Clinic in the 1930s exposed him to modern surgical methods and broadened his horizons, preparing him for a career in which he would help define oesophageal surgery as a specialty.
Barrett’s name is most enduringly associated with Barrett’s oesophagus, though his original interpretation differed from the modern concept. In 1950 he argued that cases of columnar epithelium in the lower oesophagus represented congenital short oesophagus with intrathoracic stomach, but subsequent work by Philip Allison and Alan Johnstone clarified that the mucosa was indeed oesophageal. By 1957 Barrett himself acknowledged this evolving interpretation, and the condition became recognised as the metaplastic columnar-lined oesophagus, a precursor to adenocarcinoma. His contributions also included the first successful surgical repair of Boerhaave’s syndrome, studies on hydatid cysts of the lung (“Barrett’s technique”), and his leadership as founding surgical editor of Thorax from 1946 to 1971.
Beyond the operating theatre, Barrett was a gifted teacher, writer, and draughtsman. He illustrated his own publications with meticulous drawings, blended clinical practice with historical inquiry, and lectured widely, attracting students and colleagues with his clarity and wit. A humble man despite international recognition, he served as Vice-President of the Royal College of Surgeons, President of the Thoracic Surgeons of Great Britain and Ireland, and was appointed CBE in 1969. His blend of clinical precision, surgical courage, and scholarly reflection secured him a place among the pioneers of modern thoracic surgery.
Biographical Timeline
- Born May 16, 1903 in Adelaide, South Australia, into the Barrett family of Quaker maltsters and physicians.
- 1913 – Moved with family to England; educated at The New Beacon School.
- 1917–1922 – Attended Eton College; excelled academically, elected to the elite “Eton Society (Pop),” played cricket for the school, and gained the nickname “Pasty”.
- 1922–1925 – Studied at Trinity College, Cambridge; graduated with first-class honours in the Natural Sciences Tripos.
- 1928 – Qualified MB from St. Thomas’ Hospital Medical School, London.
- 1930 – Elected Fellow of the Royal College of Surgeons (FRCS).
- 1931 – Awarded MChir, Cambridge; married Annabel Elizabeth Warington Smyth (“Betty”), a novelist.
- 1935 – Appointed Consultant Surgeon, St. Thomas’ Hospital; Rockefeller Travelling Fellowship to the United States, working at the Mayo Clinic and visiting Boston, St. Louis, and Michigan.
- 1938–1970 – Surgeon to King Edward VII Sanatorium, Midhurst, Sussex.
- 1944–1970 – Consulting Thoracic Surgeon to the Royal Navy and the Ministry of Social Security.
- 1946 – First surgical editor of Thorax (1946–1971); Published on spontaneous rupture of the oesophagus (Boerhaave syndrome), describing its dramatic and lethal presentation
- 1947 – Performed first successful repair of a ruptured oesophagus; Published on pulmonary hydatid cysts, describing his technique of enucleation without aspiration (“Barrett’s technique”).
- 1950 – Published definition of the oesophagus as squamous-lined, attributing columnar epithelium to congenital shortening with stomach displacement; the controversy over “Barrett’s oesophagus” followed.
- 1962 – President, Thoracic Surgeons of Great Britain and Ireland.
- 1962–1974 – Council member, Royal College of Surgeons (Vice-President 1972).
- 1963 – Visiting Professor of Surgery, Royal North Shore Hospital, Sydney.
- 1964 – Diagnosed with Parkinson’s disease.
- 1969 – Appointed Commander of the Order of the British Empire (CBE).
- 1970 – Retired from clinical practice.
- Died January 8, 1979 in London, aged 75.
Medical Eponyms
Barrett oesophagus (1948-1970)
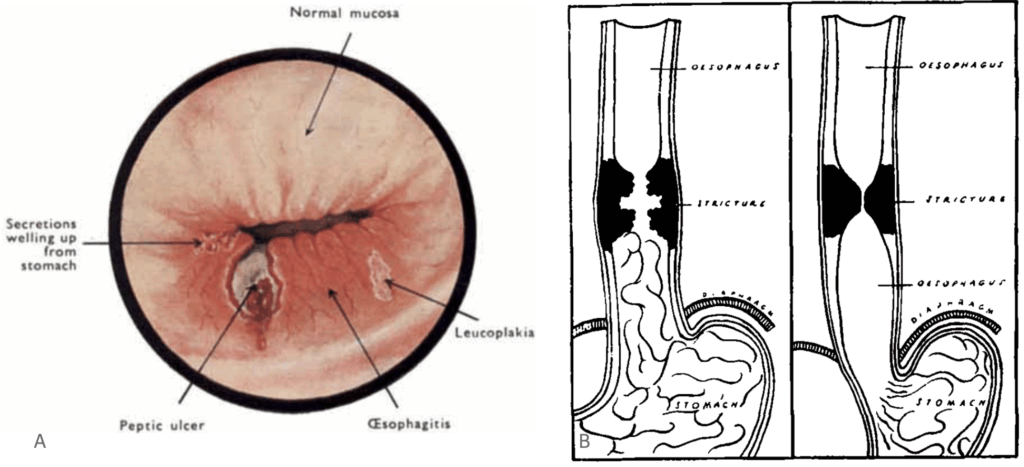
The replacement (metaplasia) of oesophageal mucosa (squamous epithelium) by gastric mucosa (columnar epithelium) by repetitive insults of refluxing gastric contents. Barrett’s oesophagus remains a pivotal concept in gastroenterology as the precursor lesion to oesophageal adenocarcinoma.
1950 – Barrett published Chronic Peptic Ulcer of the Oesophagus and ‘Oesophagitis‘. Although eponymously remembered for Barrett’s oesophagus, his original interpretation was not entirely accurate. Barrett drew a sharp distinction between reflux oesophagitis and what he believed were true congenital anomalies of the oesophagus.
Barrett described the oesophagus as “that part of the foregut, distal to the cricopharyngeal sphincter, which is lined by squamous epithelium”. Finding columnar mucosa in this region, he attributed it to a congenitally shortened oesophagus with stomach extending into the chest. He argued that many so-called “peptic ulcers of the oesophagus” were in fact ulcers of a stomach pouch drawn into the mediastinum by a congenitally short oesophagus.
I stress that the word ‘oesophagitis’ is now a blunderbuss term used to cover many different pathological lesions; it should always be qualified by a descriptive adjective such as ‘reflux oesophagitis’. I believe that reflux oesophagitis is common and that it can give rise to ulceration of the oesophagus and stricture formation. In contrast with this lesion is another which has always up till now been assumed to be identical with it, and which has generally been described by pathologists, as opposed to clinicians, under the heading of ‘peptic ulcer of the oesophagus’.
I submit that most of these cases are in truth examples of congenital short oesophagus, in which there is neither general inflammation nor stricture formation, but in which a part of the stomach extends upwards into the mediastinum – or even to the neck-and that in this stomach a typical chronic gastric ulcer can form. I urge that, as accurate surgery must rest upon accurate pathology, we must distinguish between gastric and oesophageal ulcers.
Barrett, 1950
1953 – Philip Rowland Allison (1907-1974) and Alan Stewart Johnstone (1905–1990) reviewed cases of “oesophagus lined with gastric mucous membrane,” distinguishing reflux oesophagitis from true gastric-type ulcers within the oesophagus, and suggested the term “Barrett’s ulcer” for clarity.
1957 – Barrett no longer insisted upon the congenital short oesophagus theory, instead acknowledging that the columnar-lined oesophagus represented a distinct clinical entity prone to ulceration and carcinoma.
1970 – Bremer, Lynch and Ellis were able to prove that it was not the spreading of gastric mucosa upwards but the metaplasia of squamous epithelium to columnar epithelium.
Barrett’s Technique (Pulmonary Hydatid Cysts, 1947)
In 1947, Barrett published The Treatment of Pulmonary Hydatid Disease in Thorax, describing his innovative approach to managing pulmonary hydatid cysts. Based on 30 patients with 38 lung cysts seen between 1935 and 1946 in England and Wales, Barrett carefully analysed both surgical and conservative strategies.
Rejecting aspiration and drainage due to the risks of spillage, anaphylaxis, and secondary implantation, he advocated enucleation of simple univesicular cysts without aspiration, a method later known as Barrett’s technique. His guiding principle was to remove the parasite intact, thereby minimizing contamination of the pleural cavity and improving recovery.
This paper is based upon 30 patients who suffered from pulmonary hydatid disease… A technique for the removal of simple univesicular cysts from any part of the lung is described, and the arguments for and against every step of the operation are discussed.
Barrett 1947
This surgical strategy became influential, particularly in regions where hydatid disease was endemic, and demonstrated Barrett’s characteristic blend of careful observation and practical innovation.
Key Medical Contributions
Boerhaave’s Syndrome and Oesophageal Surgery
Barrett’s expertise in thoracic surgery extended beyond his eponym. In 1946, he published a paper on spontaneous rupture of the oesophagus (Boerhaave’s syndrome) in the first issue of Thorax, famously remarking:
In the byways of surgery there can be few conditions more dramatic in their presentation and more terrible in their symptoms than spontaneous perforation of the oesophagus. No case has yet been treated successfully, and diagnosis has only been achieved in a very few before death.
Barrett, 1946
In 1947, Barrett published a case of spontaneous perforation of the oesophagus successfully treated by operation the first successful surgical repair of oesophageal rupture, transforming management of a previously universally fatal condition.
Editorial and Professional Leadership
Barrett combined surgical innovation with a passion for scholarship and teaching. From 1946 to 1971, he served as founding surgical editor of Thorax, where he cultivated its reputation for clarity and rigor. He lectured widely, drawing large audiences of students and trainees with his precision and wit.
He was President of the Thoracic Surgeons of Great Britain and Ireland (1962), Vice-President of the Royal College of Surgeons (1972), and held honorary memberships in many international societies.
Major Publications
- Barrett NR, Wheaton CEW. The pathology, diagnosis, and treatment of congenital diaphragmatic hernia in infants. The British Journal of Surgery. 1933 21,420–433.
- Barrett NR. Examination of sputum for malignant cells and particles of malignant growth. J Thorac Surg. 1938;8:169-83
- Barrett NR. Spontaneous Perforation of the Oesophagus; review of the literature and report of three new cases. Thorax. 1946 Mar;1(1):48-70.
- Barrett NR. The treatment of pulmonary hydatid disease. Thorax. 1947 Mar;2(1):21-57.
- Barrett NR. Report of a case of spontaneous perforation of the oesophagus successfully treated by operation. Br J Surg. 1947 Oct;35(138):216-8.
- Barrett NR. Chronic peptic ulcer of the oesophagus and ‘oesophagitis’. Br J Surg. 1950 Oct;38(150):175-82.
- Barrett NR. The lower esophagus lined by columnar epithelium. Surgery. 1957 Jun;41(6):881-94.
References
Biography
- Obituaries. Norman R. Barrett, CBE, MA, MChir, FRCS. St. Thomas’s Hospital gazette 1979; 77: 53-55.
- Lord RV. Norman Barrett, “doyen of esophageal surgery”. Ann Surg. 1999 Mar;229(3):428-39.
- Van den Tweel JG. Barrett, Norman (1903–1979) In: Pioneers in Pathology. 2017: 57-59
- Biography: Barrett, Norman Rupert (1903-1979). Plarr’s Lives of the Fellows Online. Royal College of Surgeons of England.
Eponymous terms
- Mackenzie M. Acute oesophagitis. In: Diseases of the throat and nose. 1884: 41-49
- Allison PR. Peptic ulcer of the esophagus. J Thorac Surg. 1946 Oct;15:308-17.
- Allison PR. Peptic ulcer of the oesophagus. Thorax. 1948 Mar;3(1):20-42
- Barrett NR. Chronic peptic ulcer of the oesophagus and ‘oesophagitis’. Br J Surg. 1950 Oct;38(150):175-82.
- Allison PR, Johnstone AS. The oesophagus lined with gastric mucous membrane. Thorax. 1953 Jun;8(2):87-101. [Describing Barrett’s Ulcer]
- Pleskow DK, Erim T. Barrett’s Esophagus: Emerging Evidence for Improved Clinical Practice. 2016
Eponym
the person behind the name
Graduated Medicine in 2020 from Queens University Belfast. Interested in Internal Medicine.
BA MA (Oxon) MBChB (Edin) FACEM FFSEM. Emergency physician, Sir Charles Gairdner Hospital. Passion for rugby; medical history; medical education; and asynchronous learning #FOAMed evangelist. Co-founder and CTO of Life in the Fast lane | On Call: Principles and Protocol 4e| Eponyms | Books |

