Obturator nerve lesions
Obturator nerve lesions cause impaired thigh adduction and medial thigh sensory loss, most often from pelvic trauma, compression, or compartment syndrome.
Obturator nerve lesions are uncommon. They manifest as:
- Inability to adduct the leg
- Variable loss of sensation on the inner aspect of the thigh
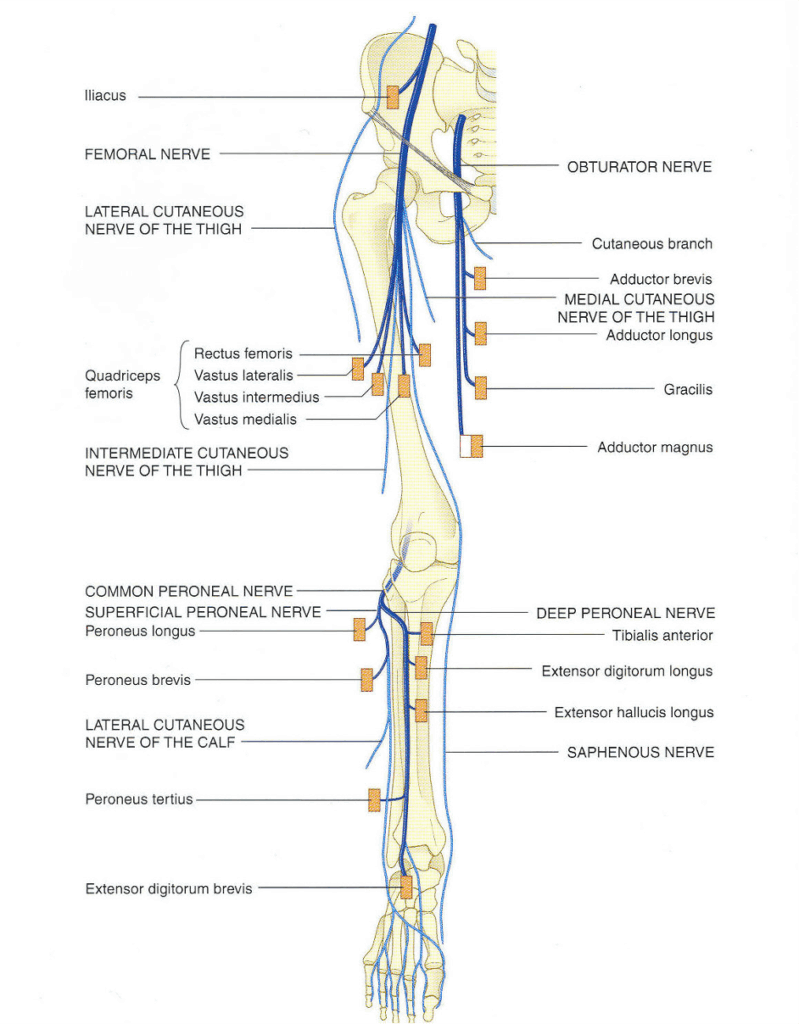
Anatomy
Course of the obturator nerve
- Derived from L2, L3, L4 nerve roots
- Arises from the lumbar plexus
- Travels down the medial border of the psoas muscle (femoral nerve travels lateral)
- Enters the obturator foramen, dividing into anterior and posterior branches
Anterior division:
- Passes through the adductor canal with obturator vessels
- Runs behind pectineus and adductor longus, in front of adductor brevis
- Terminates as a sensory nerve to the medial thigh
Posterior division:
- Pierces obturator externus
- Passes behind adductor brevis and in front of adductor magnus
- Enters adductor canal and ends as a sensory branch to the knee joint
Obturator nerve innervations
Anterior division:
- Gracilis – adducts thigh, flexes knee
- Adductor brevis – adducts thigh
- Adductor longus – adducts thigh
- Sensory branch to medial thigh
Posterior division:
- Obturator externus – laterally rotates thigh
- Adductor magnus (adductor part) – adducts thigh
- Sensory branch to knee joint
Pathology
Causes of obturator nerve lesions
- Trauma
- Typically associated with pelvic fractures
- Neuropraxias
- Compression between fetal head and bony pelvis
- Malposition of lower limb
- Entrapment in adductor magnus (athletes)
- Compartment syndrome of medial thigh
- Mass lesions
- Tumours
- Abscesses
- Neuropathies
- Rarely affect obturator nerve
- Consider diabetes, malignancy, infections, autoimmune causes if part of mononeuritis multiplex
Clinical assessment
In severe injuries:
- Loss of adduction and internal rotation
- Gait disturbance: externally rotated foot

Right: Testing motor function: The patient is asked to extend the knee and adduct the leg against the resistance of the examiner. The muscle bellies of the adductor muscles can be felt to contrac
Investigations
Blood tests (based on clinical suspicion):
- FBC
- U&Es / glucose
- CRP
- ESR
- Others as indicated (e.g., lead levels)
CT scan – to assess for mass lesions
MRI – can visualise mass lesions and nerve involvement
Management
- Treat underlying cause
- Neuropraxias
- Fasciotomy for compartment syndrome
- Occupational therapy
- Splinting and support
- Physiotherapy
- Recovery support or prevent secondary complications
Disposition
Disposition depends on:
- Cause of lesion
- Severity of symptoms
- Acuteness of onset
Appendix 1
References
Publications
- Brazis PW, Masdeu JC, Biller J. Localization in Clinical Neurology. 8e 2021
- Fuller G. Neurological Examination Made Easy. 6e 2019
- O’Brien M. Aids to the Examination of the Peripheral Nervous System. 6e 2023
FOAMed
- Coni R. Neuro 101: Peripheral Nervous System. LITFL
- Nickson C. Myotomes and Differentiating Nerve Lesions. LITFL
Fellowship Notes
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner
Educator, magister, munus exemplar, dicata in agro subitis medicina et discrimine cura | FFS |


