Oesophageal Doppler
OVERVIEW
- Oesophageal Doppler Cardiac Output Monitor
USES
- non-invasive cardiac output monitor
Contra-indications
- IABP
- severe coarctation
- known pharyngo-oesophageal pathology or injury
- oesphagectomy
- severe bleeding
- awake patient (relative)
Indications
- major surgery with large fluid/blood shifts
- high risk patients
- haemodynamic instability
DESCRIPTION
- measures blood flow velocity in the descending aorta using a flexible ultrasound probe
- measurement is based on the Doppler Principle: a doppler shift in frequency occurs when the ultrasound wave is reflected back from moving RBCs, with the shift in frequency proportional to the velocity of the blood flow
- measurement is combined with the cross-sectional area of the descending aorta (using a nomogram based on age, weight and height — some models measure aortic root diameter using TOE)
- probe contains crystals that produce a continuous ultrasound wave of 4 MHz
- single use, latex-free, silicone-based
METHOD OF INSERTION AND/OR USE
- lubricate probe well
- inserted via the nasal or oral route
- advanced and rotated in the oesophagus (typically sits at level of the 5th and 6th thoracic vertebrae where the aorta is adjacent and parallel to the oesophagus)
- some devices display the aortic pressure waveform allowing confirmation of optimal probe position
- turn volume up initially (sharpest sound = best position)
- input age, height and weight
- insert probe to 35-40cm from teeth (T5/6)
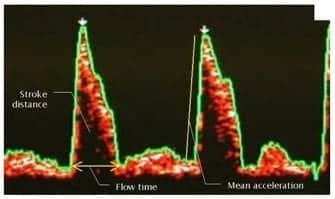
- manipulate probe until characteristic Doppler signal found (well defined triangle with black centre surrounded by red with white in trailing edge) = distribution of RBC velocities at a given point in time
- adjust cycle length (5 = good starting point), gain (to decrease ambient noise, start at 5 also)
- the brighter (whiter) the colour the greater the number of RBCs travelling at the given velocity
- it is a dynamic monitor so needs refocusing prior to each reading
INFORMATION OBTAINED
Haemodynamic parameters:
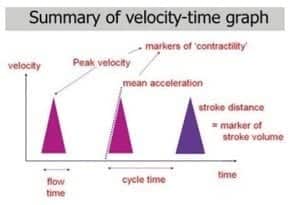
- cardiac output (Q = SV x HR)
— Q is estimated by minute distance - stroke volume (SV is dependent on preload, afterload and contractility)
— SV is measured by stroke distance x aortic root diameter
— stroke distance (AUC) x HR, linear cardiac output parameter, distance moved by a column of blood through aorta in 1 minute (1200cm = high flow state) - corrected (systolic) flow time (FTc)
— indicates preload
— normal = 0.33-0.36s
— interpretation of FTc and PV indicates afterload - peak velocity (PV)
— indicates contractility
— normal range is age related (20yrs 90-120 cm/sec, 90 yrs 30-60 cm/sec)
— interpretation of FTc and PV indicates afterload - heart rate
Actions from readings (need to be interpreted in clinical context)
- low SV -> fluid
- low FTc -> fluid
- low PV -> inotrope
- low PV + low FTc -> decrease afterload
PROS AND CONS
Advantages
- minimally invasive
- provides real time measurements
Disadvantages
- learning curve (significant inter and intra-observer variability)
- probe displacement requiring repositioning
- difficult to use in an awake patient
Complications
- esophageal bleeding, ulceration, or perforation
- stricture formation
- inaccurate measurements from probe displacement
OTHER INFORMATION
- Doppler equation: Fd= 2FtVCos θ / C
- where Ft is the transmitted Doppler frequency, V is the speed of blood flow, Cos θ is the Cosine of the blood flow to beam angle and C is the speed of sound in tissue
- perioperative use in the UK is supported by NICE guidelines and is embedded in ‘enhanced recovery after surgery’ (ERAS) programmes with financial incentives – this based largely on the surrogate outcome of reduced hospital length of stay
References and Links
- Morris C. Oesophageal Doppler monitoring, doubt and equipoise: evidence based medicine means change. Anaesthesia. 2013 Jul;68(7):684-8. PMID: 23672246.

Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC