Pelligrini-Stieda lesion
Description
Pellegrini-Stieda lesions are ossifications in or near the tibial collateral ligament (medial femoral collateral ligament) adjacent to the margin of the medial femoral condyle. Ossified post-traumatic lesions (presumed secondary to Stieda fracture)
Stieda fracture: bony avulsion injury of the medial collateral ligament at the medial femoral condyle. Calcification may form a few weeks following the initial injury (Pellegrini-Stieda lesion).
Pellegrini-Stieda syndrome: most patients are asymptomatic, however a small proportion present with medial knee pain following previous medial collateral ligament injury and Pellegrini-Stieda lesion
Imaging
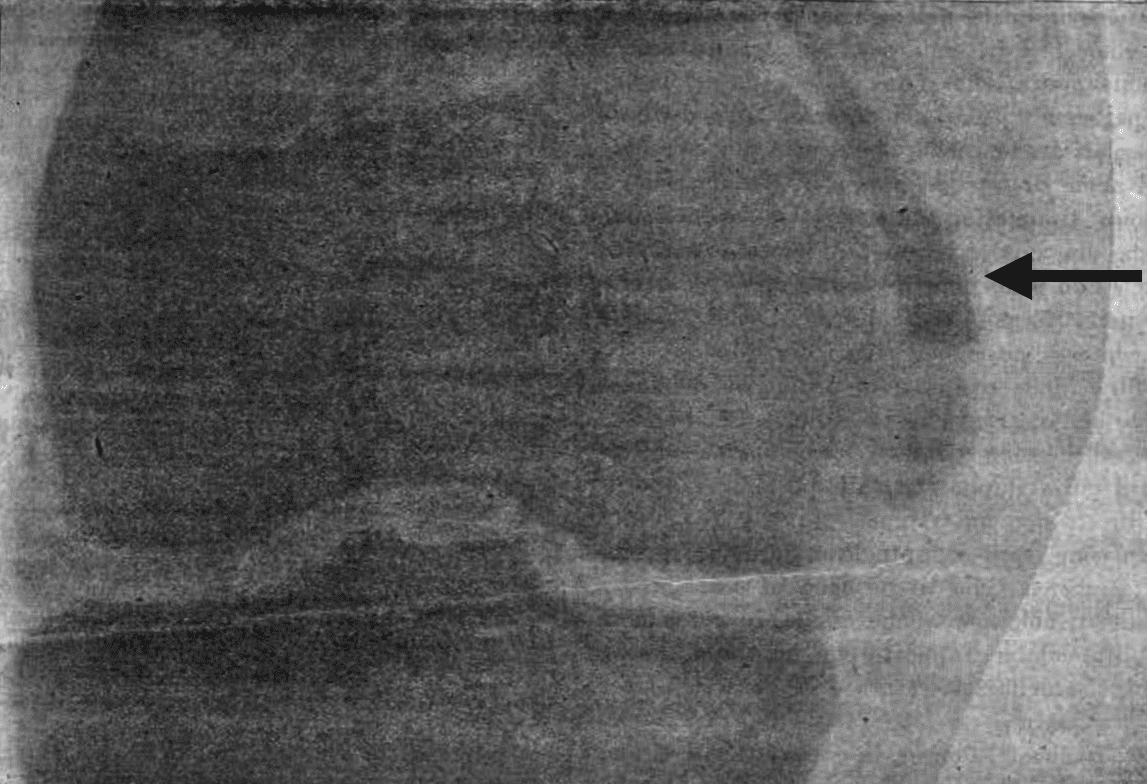
Knee X-ray: Calcification adjacent to the medial femoral condyle, often linear or curvilinear in shape and parallelling the femoral cortex.
MRI: Pellegrini-Stieda lesion appears as an ossicle or enthesophyte with bone marrow signal at the medial femoral condyle. The medial collateral ligament is usually thickened.
Management
Treatments for mild and moderate cases of the Pellegrini–Stieda syndrome include local corticosteroid injection and range-of-motion exercises. Surgical excision of calcifications and repair of the tear in the medial collateral ligament can be considered for refractory cases
History of the Pelligrini-Stieda lesion
1903 – Alban Köhler reported a case of a 56-year-old male who injured his knee during piling of wood in 1903 (published 1905)
56 jähr. Mann. Vor 4 Jahren beim Holzaufstapeln verschüttet. Verrenkung des Hüftgelenks, Kontusion des Kniegelenks… seither keine Beschwerden in der Hüfte, aber immer im Knie, wenig beim langsamen Gang, Stechen beim schnelleren Gehen und Tragen von Lasten.
Radiogramm: Am aüsseren Condylus (im Schatten) knopfförmige kompakte Hervorwölbung, ebenso aussen an Tibia. Am inneren Condylus oben am Übergang in den Schaft im Schatten der Weichteile ein kleiner flacher dunkler Schatten, im Röntgenogramm gerade oben noch zu erkennen, der nur einer bindegewebigen Ossifikation entsprechen kann.
Köhler Plate VII, Fig 12 p140
56 year old man. Injured 4 years ago whilst piling wood. Sprained hip and contusion of the knee joint … since then no complaints in the hip, but ongoing pain in the knee, minimal with slow walking, but stabbing when walking at pace, or carrying loads.
Radiograph: At the outer condyle (in the shadow) a button-shaped, compact protrusion, similarly at the outer Tibia. At the inner condyle, up at the transition to the shaft, in the shadow of the soft tissue, a small, flat, dark shadow, only just discernable on the image, which must correspond to a connective tissue ossification.
Köhler Plate VII, Fig 12 p140

1905 – Augusto Pellegrini called attention to a traumatic ossification of the collateral tibial ligament of the knee. He reported case of calcification, involving the collateral ligament of the knee in a 36-year-old man who fell at work from a height of 2 m striking the internal knee surface on an iron vessel on October 6, 1904.
Pellegrini examined him on March 13th 1905 at the Department of Surgery in Florence and concluded that the cause of ossification in the present case to have resulted from a singular traumatic event. Pellegrini pointed out that the anatomical origin of the ossification, as found upon surgery, lay at the origin of the MCL.
X-ray examination of the affected area reveals a shadow of the perfectly normal distal end of the femur and proximal end of the tibia; the tumour produces a light shadow which is just perceptible at the base of the soft parts: it is located laterally to the MCL of the femur, following its boundaries and becoming separated for a short distance; some discontinuity is perceivable in the shadow close to the distal end of the tumour; the separate portion of the tumour manifests a less intense shadow than the remainder.
Pellegrini 1905
This received minimal international attention as the journal (La Clinica moderna (Firenze)) was taken out of production shortly after his publication
1907 – Alfred Stieda, unaware of the previous work, again called attention to a semilunar-shaped calcification seen about the superior border of the internal (medial) epicondyle of the distal femur.
Stieda published 5 male cases, aged 20-48 years, post-traumatic injury with knee radiograph findings of bony shadows around the superior femoral medial epicondyle in a 1908 publication. On cadaveric dissection, he found the lesion to be situated at the origin of the medial head of the gastrocnemius.
…it undoubtedly concerns a rupture of the upper part of the internal epicondyle, and in our clinically observed cases, we may also well suppose an analog injury, especially since the position of the shadow in the X-ray fits more with a tear of the muscle insertion (upper portion of the internal epicondyle) than with a tear of the insertion of the inner sideband (lower portion of the internal epicondyle). Further, whether the projection comes off by direct force or because of muscle pull is an interesting question.
Stieda 1908

2006 – Mendes et al found that ossification in Pellegrini-Stieda disease was not confined to the Tibial Collateral ligament (TCL) but may also involve the adductor magnus tendon; and that PS disease should not be regarded as synonymous with ossification of the TCL.
They proposed that the ossification could be classified into four types indicating various potential sites of ossification post trauma; they did not find any clinical differences in the four types of ossification patterns.

2008 – McAnally et al presented four cases of four magnetic resonance imaging cases of knee trauma with complete posterior cruciate ligament tear or avulsion. They concluded that classic XR findings of Pellegrini-Stieda ossifications can be caused by stripping of the femoral periosteum proximal to the femoral attachment of the medial collateral ligament, when associated with a complete posterior cruciate ligament injury.
2017 – Somford et al reviewed the original differences in the original descriptions of Pellegrini and Stieda and follow the vision on the origin of the lesion over time. After PubMed review they identified almost 5000 articles, and formally reviewed 37, specifically looking at the anatomical origin o fthe lesion. Proposed origins included medial collateral ligament (MCL, medial gastrocnemius, adductor magnus, vastus medialis, deep MCL, and superficial MCL. The MCL was most often coined as origin of the lesion (54% overall, 25% on MRI, and 57% during surgery), however many cases remained undetermined (50% on MRI) or no specific structure was found to be the origin (29% during surgery).
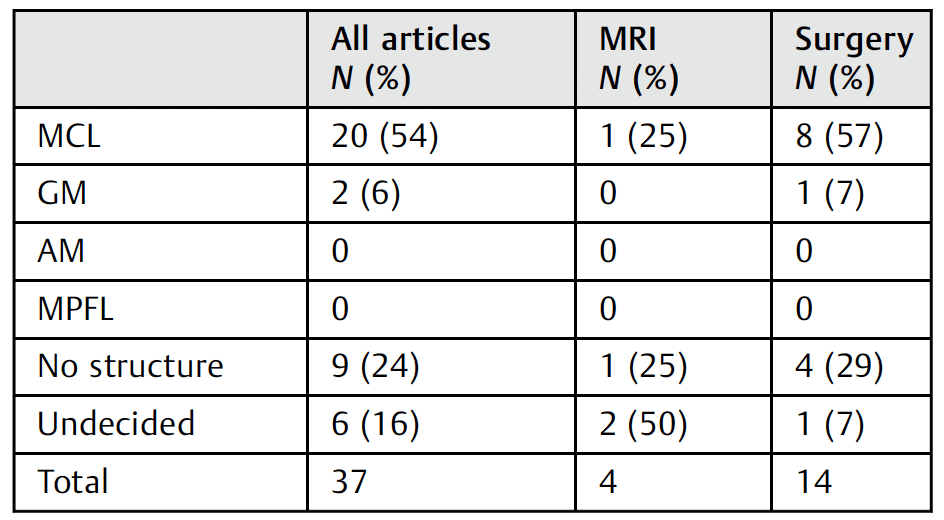
Abbreviations: AM, adductor magnus tendon; GM, medial head of gastrocnemius muscle; MCL, medial collateral ligament; MPFL, medial patellofemoral ligament; MRI, magnetic resonance imaging.
Note: Articles naming several structures are labeled undecided. Somford et al 2017
They concluded that the eponymous term Pellegrini–Stieda lesion was fitting, as it comprised two alternate anatomical origins of the lesion. MRI was deemed to be a noninvasive and quite accurate method for future research.
Associated Persons
- Alban Köhler (1874–1947)
- Augusto Pellegrini (1877-1958)
- Alfred Stieda (1869-1945)
Alternative names
- Köhler-Pelligrini-Stieda disease
- Pellegrini-Stieda disease
- Pellegrini-Stieda sign
- Stieda fracture
- Pellegrini-Stieda syndrome
- Pellegrini-Stieda phenomenon
Controversies
- Perhaps historically this lesion might be named the Köhler-Pellegrini-Stieda lesion
References
Original articles
- Köhler A. Die normale und pathologische Anatomie des Hüftgelenks und Oberschenkels in röntgenographischer Darstellung. Hamburg, Lucas Gräfe & Sillem, 1905
- Pellegrini A. Ossificazione traumatica del ligamento collaterale tibiale dell’articolazione del ginocchio sinistro. [Traumatic calcification of the collateral tibial ligament of the knee joint] Clinica moderna (Firenze) 1905; 11: 433-439
- Stieda A. Uber eine typische verletzung am unteren femurende. Archiv für Klinische Chirurgie, 1908; 85: 815-826
- Vogel K. Über eine typische Fractur des Epicondylus internus femoris. Archiv für Klinische Chirurgie 1908; 87: 1077–1091. [Case series referencing Stieda]
- Odessky IM. Post-traumatic Para-articular Ossification of the Knee Joint (“Köhler-Pellegrini-Stieda Shadow”). Radiology. 1934; 22(6): 701-706
Review articles
- Wang JC, Shapiro MS. Pellegrini-Stieda syndrome. Am J Orthop (Belle Mead NJ). 1995; 24(6): 493-7.
- Wiegerinck JI, Somford MP. Review of Stieda’s article (1908) on the Pellegrini-Stieda lesion. Journal of ISAKOS: Joint Disorders & Orthopaedic Sports Medicine 2016;1:214-218.
- Mendes LF, Pretterklieber ML, Cho JH, Garcia GM, Resnick DL, Chung CB. Pellegrini–Stieda disease: a heterogeneous disorder not synonymous with ossification/calcification of the tibial collateral ligament—anatomic and imaging investigation. Skeletal Radiol. 2006; 35(12): 916-22.
- Altschuler EL, Bryce TN. Images in clinical medicine. Pellegrini-Stieda syndrome. N Engl J Med. 2006; 354(1): e1.
- McAnally JL, Southam SL, Mlady GW. New thoughts on the origin of Pellegrini-Stieda: the association of PCL injury and medial femoral epicondylar periosteal stripping. Skeletal Radiol. 2009; 38(2): 193-8.
- Somford MP, Lorusso L, Porro A, Loon CV, Eygendaal D. The Pellegrini-Stieda Lesion Dissected Historically. J Knee Surg. 2018; 31(6): 562-567.
- Somford MP et al. Biographical background and origin of common eponymous terms in orthopedic surgery: anatomy and fractures in knee surgery. Eur J Orthop Surg Traumatol. 2018 Jan;28(1):79-84
- Weaver M, Sherman AI. Pellegrini Stieda Disease. StatPearls 2020
- Denq W, Ahlzadeh G. SplintER Series: Delayed pain in an injured knee. ALiEM 2020
- Haouimi A. Pellegrini-Stieda lesion. Radiopaedia
[cite]
eponymictionary
the names behind the name
Resident medical officer in emergency medicine MB ChB (Uni. Dundee) MRCS Ed. Avid traveller, yoga teacher, polylinguist with a passion for discovering cultures.


