Physiology of Pregnancy
OVERVIEW
- fetus considered viable at 24-25 weeks with a weight of > 750g
Airway
- progesterone mediated hyperaemia and oedema of mucosal surfaces -> down size tubes
- difficult -> higher incidence of failure to intubate
Breathing
- higher O2 consumption
- desaturate quickly
- increased aspiration risk
- increased risk of pulmonary oedema (increased blood volume and lower oncotic pressure)
- mechanical ventilation can be problematic
- difficult to implement protective ventilation -> hypercapnia produces fetal acidosis
- cephalad movement of diaphragm @ 37 weeks -> place chest drain higher than normal
- spirometry, flow volume loops and peak flow rates -> unchanged
- TLC decreases 5% c/o cephalad movement of diaphragm
- FRC decreases by 20% -> decreased ERV and RV
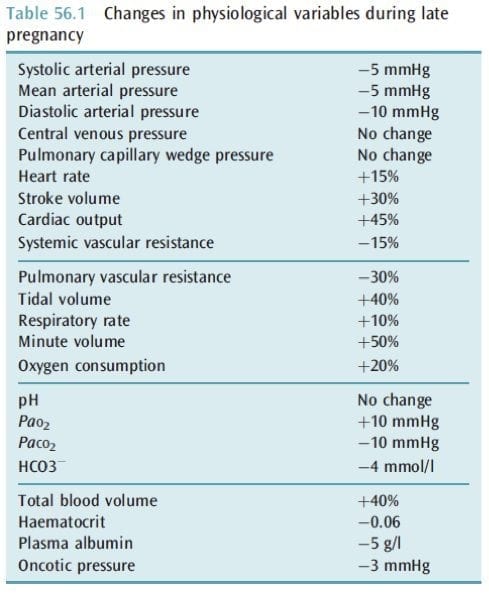
- MV increases by 50% from increase in TV -> chronic respiratory alkalosis (pH 7.4 to 7.47, PaCO2 30-32mmHg, slightly elevated PaO2, kidneys excrete HCO3- to compensate to keep HCO3- 18-21mmol/L, BE 3-4)
- O2 consumption increased 20%
Circulation
- tachycardia, low BP, increased Q and warm peripheries -> normal in pregnancy
- aortocaval compression
- PAC’s can be helpful in severe pre-eclampsia, APO and cardiac disease (non-invasive Q monitors are useless)
- uterine bed is sensitive to vasoconstrictors
- phenylephrine better than ephedrine -> less fetal acidosis
- no evidence favouring any particular inotrope
- diaphragm pushed upward and heart rotated to left -> changes Q waves inferiorly and gives TWI
- maternal blood volume increases 40%, red cell mass increases 25% -> relative anaemia of pregnancy
- normal ejection systolic murmur and third heart sound
- normal echo: increase in all cardiac chamber dimensions, increased LV thickness, small pericardial effusions, mild TR, mild MR
Coagulation
- x 5 increased in VTE -> prophylaxis is important
Gastrointestinal
- GORD -> aspiration
- hypoalbuminaemia from haemodilution
- increase in ALP
- appendicitis and cholecystitis happen
Genitourinary
- at 12/40 bladder becomes an abdominal structure -> susceptible to blunt trauma
- at 20/40 fundus at umbilicus -> susceptible to blunt or penetrating trauma
- GFR increases by 50% -> lower Cr, urea, uric acid
Placenta
- uterine blood flow @ term = 10% (600-700mL/min)
- under stress maternal blood flow will be maintained at the expense of the fetus
- oxygen consumption = 20mL/min -> can survive 10 min by shunting blood flow to vital organs and decreasing O2 consumption.
(TIME) -> its like the liver, kidney & the lungs all in one!
Transport
- gas exchange (O2 & CO2) – fetal Hb (higher concentration, greater affinity for O2)
- delivery of nutrients (glucose, aa, lipids)
- removal of wastes (urea, bilirubin)
- transport of other substances (drugs)
- heat transfer
Immunological
- protection of foetus from infection
- protection of foetus from rejection by mother (immunological barrier function)
- trophoblast cells do display Class I or II MHC (major histocompatibility complex) proteins thus they cannot present antigen to lymphocytes and cannot be recognised by activated cytotoxic T lymphocytes.
Metabolic
- synthesis of glycogen, cholesterol, FFA’s and enzymes
Endocrine
- synthesis of 4 main hormones: hCG, oestriol, progesterone, human placental lactogen
- synthesis of various other hormones & growth factors
Mother and Baby
- monitor for preterm labour
- think about placental transfer of drugs
- maintenance of placental perfusion and oxygenation

Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC