Refeeding Syndrome
OVERVIEW
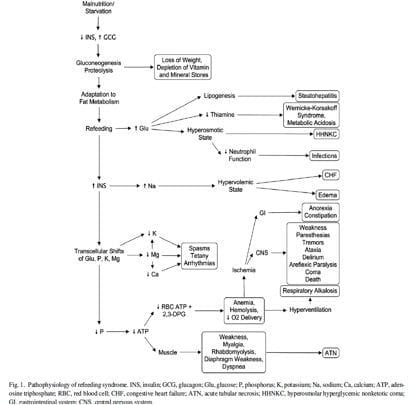
- Refeeding Syndrome = a group of clinical findings that occur in severely malnourished individuals undergoing nutritional support.
- underecognised
- occurs in the setting of prolonged starvation followed by provision of nutritional supplementation from any route.
- chronic malnutrition leads to protein catabolism with total body phosphate depletion despite normal serum phosphate
- introduction of carbohydrates leads to an anabolic state which unmasks total body phosphate depletion and leads to precipitous drop in serum phosphate
- insulin + glucose = massive uptake of phosphate, K+ and Mg2+ into cells
RISK FACTORS – anyone who may be malnourished:
Decreased intake
- eating disorders (especially anorexia nervosa)
- alcoholism
- depression
- fasting
- vomiting
- dysphagia
- chemotherapy
- prolonged NBM
- post-operative
- chronic malnutrition
Decreased absorption
- Oncology patients
- Postoperative patients
- Elderly patients (comorbidities, decreased physiological reserve)
- uncontrolled diabetes mellitus (electrolyte depletion, diuresis)
- chronic malnutrition:
- marasmus
- prolonged fasting or low energy diet
- morbid obesity with profound weight loss
- high stress patient unfed for >7 days
- Long term users of antacids (magnesium and aluminium salts bind phosphate)
- Long term users of diuretics (loss of electrolytes)
Decreased absorption
- Malabsorptive syndrome (such as inflammatory bowel disease, chronic pancreatitis, cystic fibrosis, short bowel syndrome)
Increased catabolism
- inflammatory process (infectious and non-infectious)
- cancer
CLINICAL FEATURES
- CVS: arrhythmia, HT, CHF
- GI: abdo pain, constipation, vomiting, anorexia
- MUSC: weakness, myalgia, rhabdomyolysis, osteomalacia
- RESP: SOB, ventilator dependence, respiratory muscle weakness -> requiring intubation and ventilation
- NEURO: weakness, paraesthesia, ataxia, delirium, coma, central pontine myelinosis, seizures, Korsakoff syndrome or Wernicke encephalopathy (confusion, ataxia, ophthalmoplegia)
- METABOLIC: infections, thrombocytopaenia, haemolysis, anaemia
- HAEM: reduced 2,3 DPG production -> left shift of oxyHb dissociation curve
- OTHER: ATN, Wernicke encephalopathy, liver failure
INVESTIGATIONS
- hypophosphataemia
- hypokalaemia
- hypomagnesaemia
- hyperglycaemia
- thiamine deficiency (erythrocyte transketolase or thiamine level)
- trace elements deficiencies
MANAGEMENT
Summary of Management
(1) recognize patients at risk
(2) provide adequate electrolytes, vitamin (thiamine, water and fat soluble) and micronutrient (Zn, Fe, Se) supplementation
(3) careful fluid resuscitation to avoid fluid overload
(4) cautious and gradual energy restoration
(5) monitoring of critical laboratory indices
Resuscitate
- A – may need intubation for encephalopathy and bulbar dysfunction with aspiration
- B – ventilation because of respiratory muscle weakness with hypercapnic respiratory failure
- C – correction of electrolytes c/o arrhythmias, cautious slow volume resuscitation, central access and invasive monitoring if haemodynamically unstable
- D – may have profound weakness, cerebellar dysfunction, delirium and coma -> responds to slow correction of electrolytes
Electrolyte abnormalities + Acid Base Disturbance
- Hypophosphataemia
- Hypokalaemia (<3.5mmol/L) – replace IV or PO
- Hypomagnesaemia (<0.7mmol/L) – replace IV or PO
- Hyponatraemia – don’t correct rapidly unless symptomatic (less than 10mmol/L/day)
- Hyperglycaemia – monitor -> insulin if required
Supportive care and monitoring
Underlying cause
- screen those at risk
Feed
- 100mg/day
- Vitamin B6 (pyridoxine) – 1.7mg/day
- Vitamin B12 (cobalamin) – IM injection
- Folate – 400mcg/day
- Fat soluble vitamins – DEKA – can be replaced via feed
Micronutrients
- Selenium – 100-400mcg/day LD -> 20-70mcg/day
- Zinc – 10-30mg/day LD -> 2.5-5mg/day
- Iron – no loading dose required -> 10mg/day PO
Disposition
- managed in an HDU/ICU environment if severe
References and Links
- Khan LU, Ahmed J, Khan S, Macfie J. Refeeding syndrome: a literature review. Gastroenterol Res Pract. 2011;2011. PMC2945646.
- Mehanna HM, Moledina J, Travis J. Refeeding syndrome: what it is, and how to prevent and treat it. BMJ. 2008 Jun 28;336(7659):1495-8. PMC2440847.

Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC

ASPEN came out with new adult and pediatric criteria on this matter including a new clinical definition and new screening guidelines.