RIFLE Criteria and AKIN Classification
OVERVIEW
- AKI can be defined as an abrupt (1 to 7 days) and sustained (more than 24 hours) decrease in kidney function.
- Over 30 definitions of acute renal failure/AKI have been used in the literature.
- The ADQI formulated the RIFLE criteria in 2004 to allow for AKI to be objectively and uniformly defined.
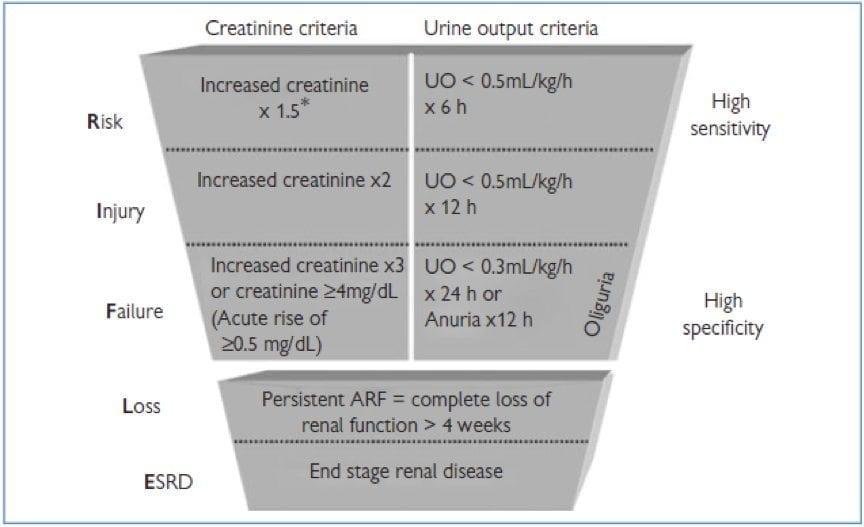
RIFLE CRITERIA
IMPLICATIONS
The implication of this classification is that a progression down the RIFLE criteria is associated with:
- increased LOS in ICU
- increased LOS in Hospital
- higher mortality
- lower renal recovery (for example, higher serum creatinine at hospital discharge)
AKI can be present with a normal creatinine, if it is sufficiently elevated above baseline.
LIMITATIONS
- Retrospective tool — need to measure changes in Cr and UO over time
- Requires baseline creatinine— ADQI recommends a creatinine estimation based on the Modification of Diet in Renal Disease (MDRD) formula, assuming a normal GFR of approximately 75 to 100 ml/min/1.73 m2 (but this may not be valid)
- Accuracy of urine output measures
- Urine output affected by many factors such as: — the use of diuretics — ADH response — diabetes insipidis
- Baseline creatinine may be affected by the patients concurrent health problem e.g. it may be falsely high purely because the patient was dehydrated on admission
- It is uncertain how well balanced urine output and creatinine are even though they have been given an equal weighting (RIFLE using creatinine have higher mortality than if using UO)
- smaller changes in creatinine than those specified under class Risk (e.g. Cr increase by 0.3 mg/dl) are associated with worse outcomes (see AKIN modifciation)
- Novel renal biomarkers, in the future, may be able to detect injury earlier
- Does not consider the nature or site of AKI
AKIN CLASSIFICATION
In 2007 the AKI Network proposed the following changes to the RIFLE criteria:
- proposed that stages 1, 2 and 3 be used instead of R, I and F; L and E are discarded
- broadening of the ‘risk’ category of RIFLE to include increase in serum creatinine of at least 0.3 mg/dl even if this does not reach 1.5x the baseline creatinine
- Cr measurements had to be measured within a 48h window (this may miss AKI that progresses more slowly) — baseline creatinine is replaced by the reference creatinine (the first Cr measured) — however it is recommended that “staging take place over a longer period (e.g. 7 days)”
- categorizing patients as ‘failure’ (stage 3) if they are treated with RRT regardless of what their serum creatinine or urine output is at the point of initiation (this may be confounding)
- GFR was discarded (used as an alternative to Cr in the original RIFLE criteria. causing additional variation based on its calculation)
- Diagnostic criteria to be used only “after an optimal state of hydration has been achieved” and “easily reversible causes” (such as urinary obstruction) should be excluded
Overall, the AKIN modification does not perform better than the RIFLE criteria in studies. Either may be used.
References and Links
- ADQI – Acute Dialysis Quality Initiative
- Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P; Acute Dialysis Quality Initiative workgroup. Acute renal failure – definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004 Aug;8(4):R204-12. PMC522841.
- Cruz DN, Ricci Z, Ronco C. Clinical review: RIFLE and AKIN–time for reappraisal. Crit Care. 2009;13(3):211. PMC2717405.
- Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, Levin A; Acute Kidney Injury Network. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007;11(2):R31. PMC2206446.
- Srisawat N, Hoste EE, Kellum JA. Modern classification of acute kidney injury. Blood Purif. 2010;29(3):300-7. PMID: 20130395.

Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC