ROSC, hypotension and an ECG exigency
aka ECG Exigency 019
A 68 year-old woman collapsed at home, as witnessed by her son who commenced CPR. She was in ventricular fibrillation when the paramedics arrived, and reverted to sinus rhythm following defibrillation at the scene. She was intubated prehospital and transferred to your emergency department. She remains intubated and unconscious, and she has a blood pressure of 75/50 mmHg.
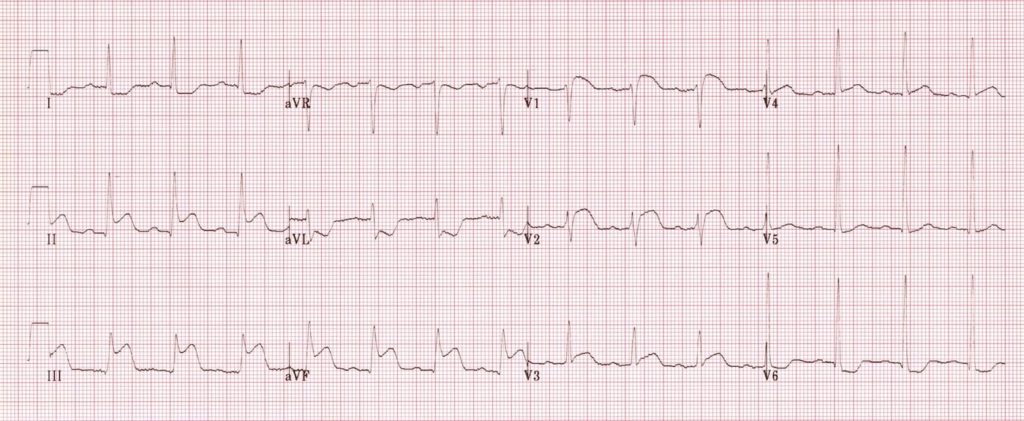
This is her ECG:
Questions
Q1. Describe and interpret the ECG.
Answer and interpretation
Description
- SR 90/min (borderline for 1st degree heart block), normal axis.
- ST elevation in the inferior leads (II, III, aVF)
- ST elevation in V1, V2 and V3
- Reciprocal ST depression in lateral leads (I, aVL and V6)
Interpretation
- Inferior STEMI with right ventricular involvement, due to acute proximal occlusion of the right coronary artery.
- Haemodynamically unstable RV infarction is associated with high mortality.
Key features suggesting RV infarction are
- ST elevation in V1
- ST elevation in lead III > lead II
Note that about one quarter to one third of inferior STEMIs are associated with RV infarction, and nearly 90% of RV infarctions occur with coexistant inferior MI.
Q2. What is the relevance of leads V1 and V2 to the diagnosis in this case?
Answer and interpretation
ST segment elevation in V1 should always make you suspect the presence of RV infarction.
The typical findings of RV infarction in V1 and V2 are:
- ST elevation in V1 exceeding the magnitude of ST elevation in V2
- ST segment in V1 is isoelectric and the ST segment in V2 is markedly depressed
These findings are not present in the ECG of our patient. Although ST elevation is usually restricted to lead V1 in RV infarction, it can occasionally extend across the precordial leads as shown in this ECG.
Q3. What can be immediately done at the bedside to confirm the diagnosis?
Q4. Describe your approach to management.
Answer and interpretation
The approach to management includes:
- Immediate activation of the cath lab.
- Employ a team-based approach to resuscitation in an appropriately equipped and staffed resuscitation area.
- Confirm ETT placement, adequacy of oxygenation (target SaO2 94-98%) and ventilation.
- Obtain large bore IV access and commence full non-invasive monitoring (SpO2, ETCO2, BP, ECG and temperature)
- Treat cardiogenic shock due to RV infarction:
— 250 mL crystalloid boluses followed by reassessment (targeting adequate end organ perfusion, usually with MAP >65 mmHg)
— maintain preload by avoiding nitrates and excessive intrathoracic pressures (e.g. avoid high PEEP)
— maintain atrio-ventricular synchrony
— transfer to the cath lab for cardiac catheterisation ASAP - Commence supportive care of the intubated patient (e.g. FAST HUGS IN BED Please!)
- Commence Targeted Temperature Management (TTM) as appropriate
This patient’s presentation is consistent with a critical right coronary artery occlusion requiring emergent reperfusion therapy. Ideally, transfer to the cath lab should occur so rapidly that there is insufficient time to do much else!
If percutaneous coronary intervention (PCI) is not available, then thrombolysis — though not as effective, particularly in the presence of cardiogenic shock — should be performed. Following thrombolysis, transfer to a facility with a cath lab is still a priority (for rescue therapy and/or further investigation).
In addition to judicious fluid boluses (to improve preload and RV function), ongoing hypotension may be treated with catecholamine infusions (e.g. dobutamine, noradrenaline), levosimendin (a calcium sensitiser), and devices such as mechanical circulatory supports (LV dysfunction may result from the inferior STEMI component) until definitive treatment can be performed. Milrinone can be a useful inodilator in RV dysfunction as pulmonary vasodilation can help decreased RV afterload. Vasopressin may also be used in preference to noradrenaline, or as a noradrenaline sparing agent, as it typically causes less pulmonary vasoconstriction than noradrenaline.
References and Links
- ECG Library — RV infarction
- Berent R, Auer J, von Duvillard S, Sinzinger H, Steinbrenner D, Schmid P. Acute myocardial infarction with ST segment elevation in inferior and anterior leads: right ventricular infarction. BMJ Case Rep. 2010;2010. pii: bcr03.2009.1700. Epub 2010 Jan 13. PubMed PMID: 22242057; PubMed Central PMCID: PMC3028157
- Walker LA, Buttrick PM. The right ventricle: biologic insights and response to disease. Curr Cardiol Rev. 2009 Jan;5(1):22-8. PubMed PMID: 20066144; PubMed Central PMCID: PMC2803284.
CLINICAL CASES
ECG EXIGENCY
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC

I am confused by:
“The typical findings of RV infarction in V1 and V2 are:
ST elevation in V1 exceeding the magnitude of ST elevation in V2
ST segment in V1 is isoelectric and the ST segment in V2 is markedly depressed
These findings are not present in the ECG of our patient. Although ST elevation is usually restricted to lead V1 in RV infarction”
This seems to provide 3 contradictory pieces of information. I’m not sure from reading this whether in RV infarction I should expect:
1. ST elevation in V1 exceeding the magnitude of ST elevation in V2
2. an isoelectric V1 and ST depression in V2
3. ST elevation in V1 and in no other leads
Any of those possibilities can be seen in RV infarction – though the classic finding in the precordial leads is STE elevation in V1 greater than in V2.
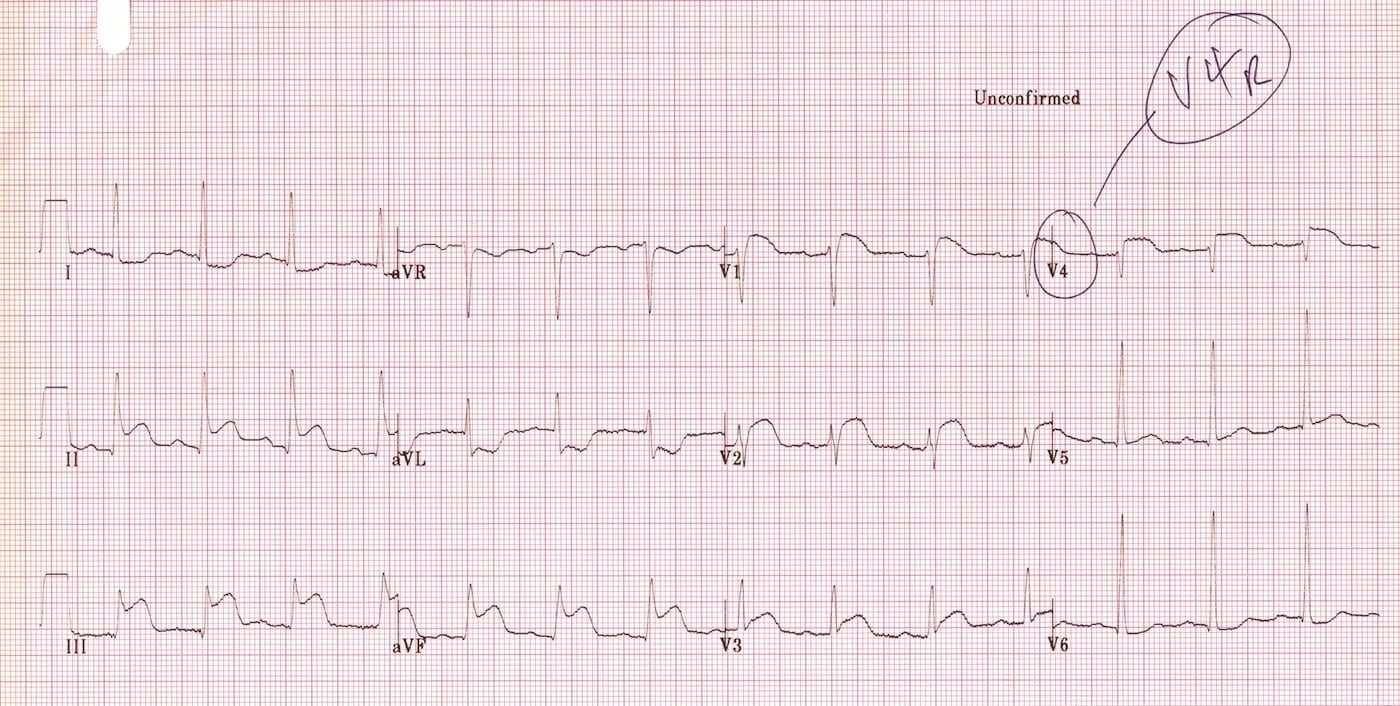
Diagnosis is confirmed by the presence of ST elevation in the right-sided leads (V3R-V6R).
Cheers
Chris
Would you really use levosimendan in the acute management of hypotension in this case, if fluid boluses didn’t do enough? My understanding is that it takes many hours to get to full effect. I’ve never commenced this in the acute setting. Should I?
Hi
Levosimendan could certainly be considered in addition to catecholamine infusions for management of cardiogenic shock.
Milrinone is an alternative, that is used more commonly in my setting – their pulmonary vasodilatory effect helps reduces RV afterload in the setting of RV failure.
Both levosimendan and milrinone can worsen hypotension through vasodilatino though – noradrenaline is often used to counter this.
Consideration of whether mechanical circulatory support devices is also warranted – though age, presence of comorbidities, and established post-arrest shock state may mean further mechanical supports are contra-indicated.
Cheers
Chris
What do you think about using Vasopressin instead of Noradrenalin in situations where lower pulmonal pressure ist desirable?
I agree that vasopressin, rather than noradrenaline is worth considering in patients with pulmonary hypertension and where you want to minimise pulmonary vasconstriction. Probably the main downside is that noradrenaline is more easily titratable in dynamic situations as it wears off rapidly. They can also be used together, with vasopressin as a noradrenaline sparing agent but still have the option of rapidly titrating noradrenaline if needed.
Would giving fluid bolus increase the filling pressure in the RV, knowing that RV infarction will lead to poor contractility?
Wouldnt the first option to maintain cardiac output in this case be inotropes?
Great case!
Judicious fluid boluses (e.g. 250 mL) and monitoring for response are reasonable, especially while getting lines in. Some patients stabilise without need for inotropes. Frequent reassessment is needed to try to ensure optimal filling for contraction (sweet spot on the Starling curve) avoid flooding the patient. Of note, infarcted heart muscle may be non-contractile and may not respond to inotropic support.