Right Ventricular Infarction
Suspect and look for right ventricular (RV) infarction in all patients with inferior STEMI.
ECG diagnostic criteria
In patients with inferior STEMI, RV infarction is suggested by:
- ST elevation in V1
- ST elevation in V1 and ST depression in V2 (highly specific for RV infarction)
- Isoelectric ST segment in V1 with marked ST depression in V2
- ST elevation in III > II
Diagnosis is confirmed by the presence of ST elevation in the right-sided leads (V3R-V6R)
- V1 is the only standard ECG lead that looks directly at the right ventricle
- Lead III is more rightward facing than lead II and hence more sensitive to the injury current produced by the right ventricle
Clinical Significance of RV Infarction
- RV infarction complicates up to 40% of inferior STEMIs (isolated RV infarction is extremely uncommon)
- These patients are very preload sensitive (due to poor RV contractility) and can develop severe hypotension in response to nitrates or other preload-reducing agents.
- Hypotension in right ventricular infarction is treated with fluid loading, and nitrates are contraindicated.
The ECG changes of RV infarction are subtle and easily missed!
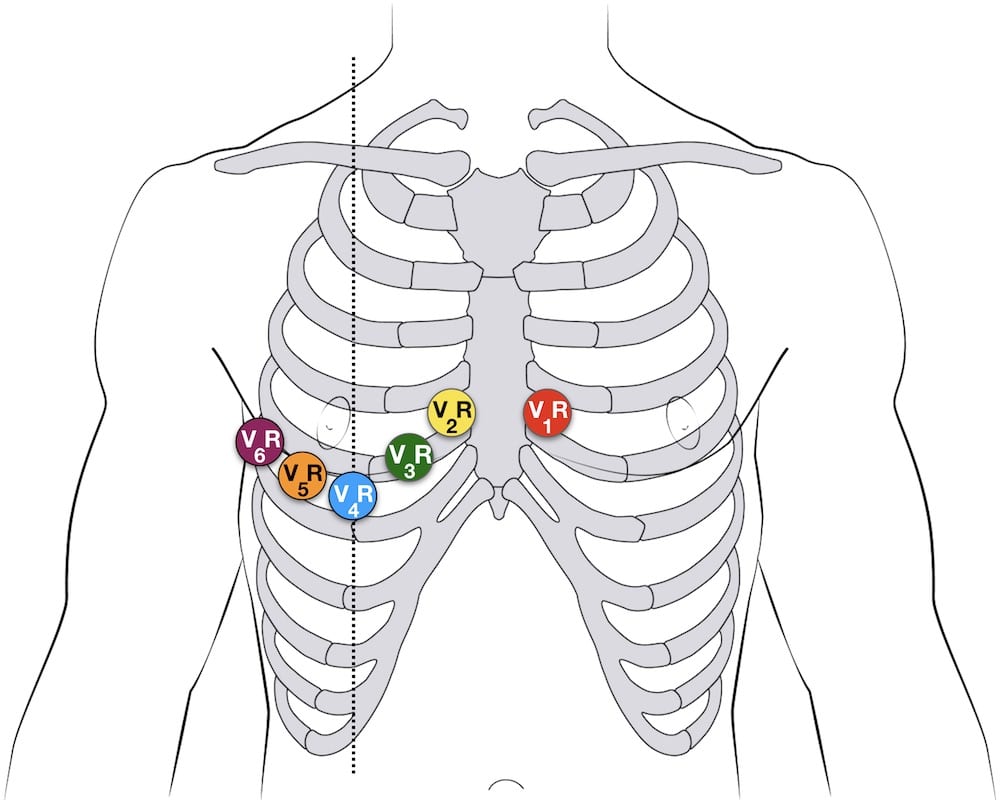
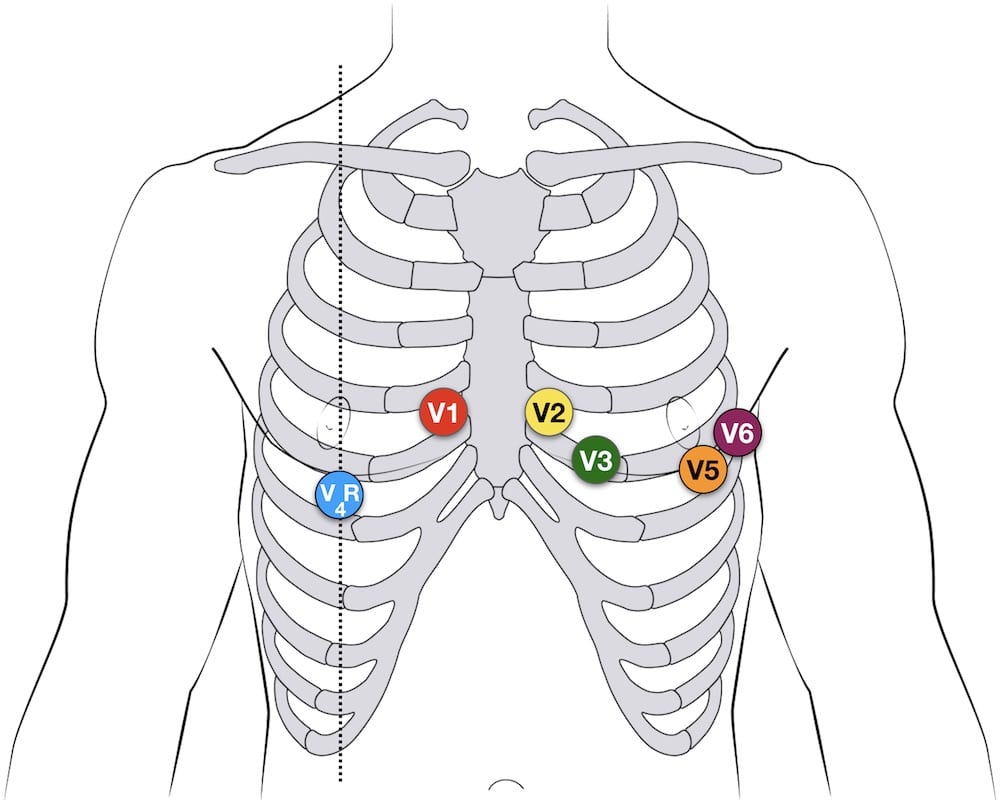
Right-sided leads
There are several approaches to recording a right-sided ECG:
- A complete set of right-sided leads is obtained by placing leads V1-6 in a mirror-image position on the right side of the chest (see diagram below)
- It may be simpler to leave V1 and V2 in their usual positions and just transfer leads V3-6 to the right side of the chest (i.e. V3R to V6R)
- The most useful lead is V4R, which is obtained by placing the V4 electrode in the 5th right intercostal space in the mid-clavicular line
- ST elevation in V4R has a sensitivity of 88%, specificity of 78% and diagnostic accuracy of 83% in the diagnosis of RV MI
NB. ST elevation in the right-sided leads is a transient phenomenon, lasting less than 10 hours in 50% of patients with RV infarction.
Example ECG
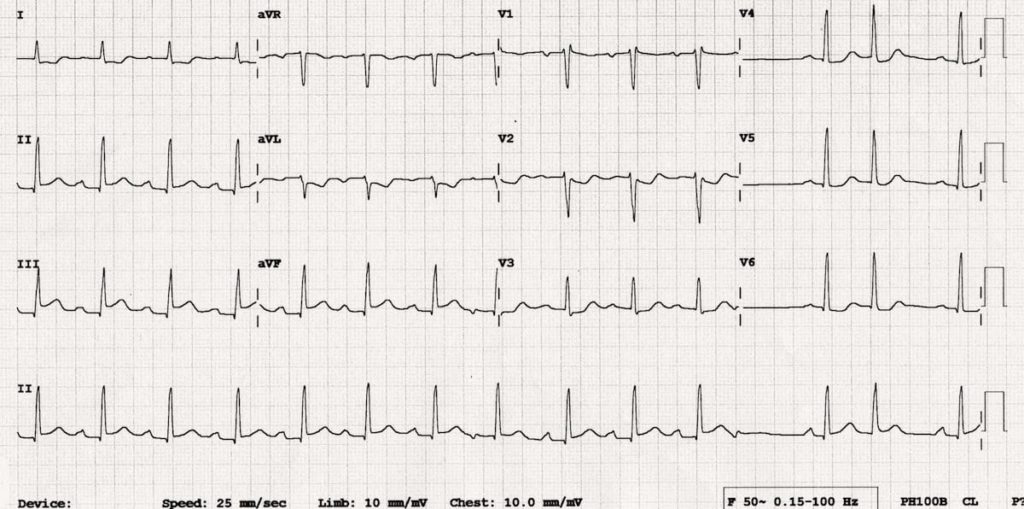
Example 1a
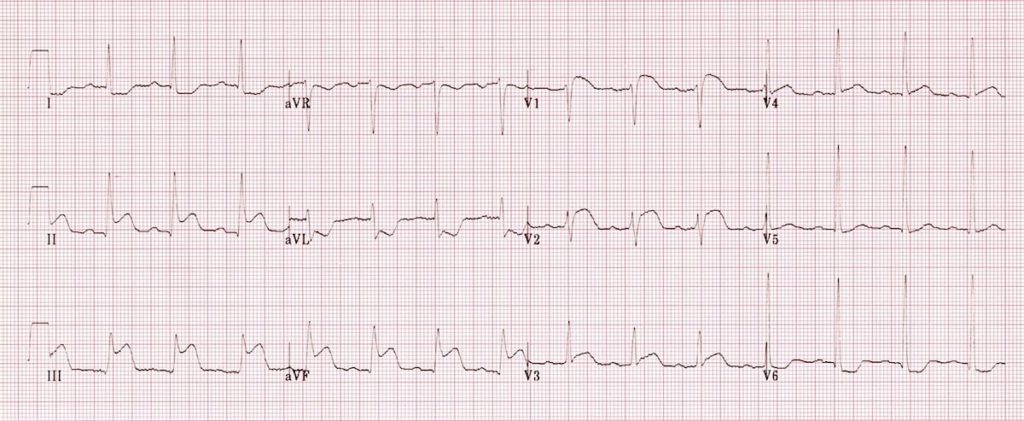
Inferior STEMI. Right ventricular infarction is suggested by:
- ST elevation in V1
- ST elevation in lead III > lead II
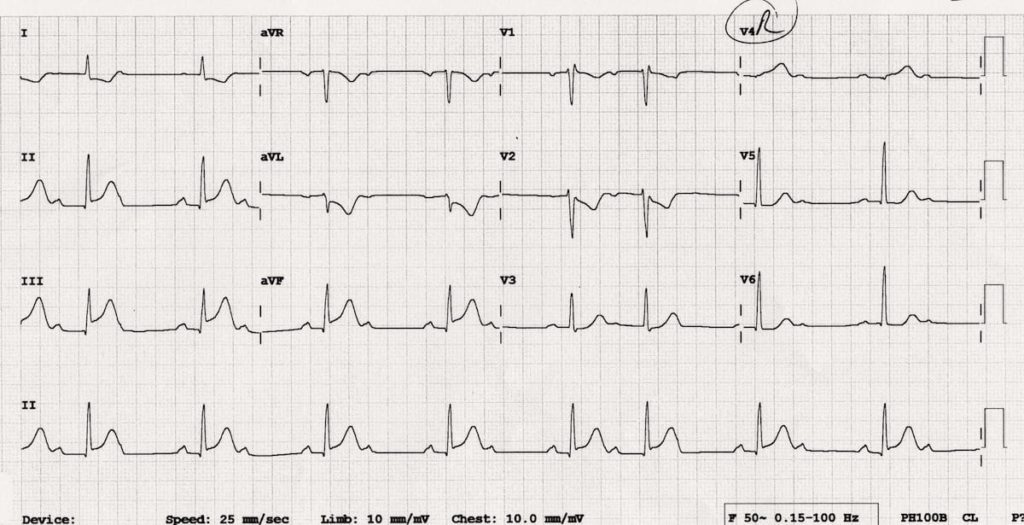
Example 1b
Repeat ECG of the same patient with V4R electrode position:

- There is ST elevation in V4R consistent with RV infarction
Example 2

Another example of right ventricular infarction in the context of inferior STEMI:
- ST elevation in lead III > lead II
- Isoelectric ST segment in V1 with marked ST depression in V2
- There is ST elevation in V4R.
Example 3
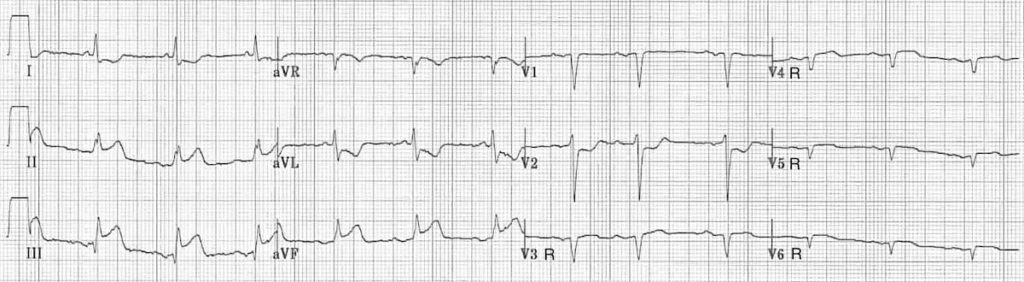
This ECG shows a full set of right-sided leads (V3R-V6R), with V1 and V2 in their original positions. RV infarction is diagnosed based on the following findings:
- There is an inferior STEMI with ST elevation in lead III > lead II
- V1 is isoelectric while V2 is significantly depressed
- There is ST elevation throughout the right-sided leads V3R-V6R
Example 4a
Try this one yourself…
Reveal Interpretation
- Inferior STEMI with STE in III > II
- Reciprocal ST depression in aVL and I
- Isoelectric ST segment in V1 with ST depression in V2-3
- These findings are consistent with inferior STEMI due to RCA occlusion, plus likely associated RV infarction.
Example 4b
Same patient, 9 minutes later…
Reveal Interpretation
- Rapid evolution of inferior STEMI with dynamic increase in height of ST segments – this patient needs urgent PCI!
- V4R shows loss of R-wave height, significant ST elevation (> 0.5mm; ST segment > R wave) and hyperacute T wave (very large T wave given amplitude of QRS complex) – this confirms the diagnosis of RV MI
- Development of Wenckebach 2nd degree AV block indicates AV nodal ischaemia or a Bezold-Jarisch reflex (increased vagal tone often seen with inferior MI)
Related Topics
References
- Morris F, Brady WJ. ABC of clinical electrocardiography: Acute myocardial infarction-Part I. BMJ. 2002; 324: 831-4. [full text]
- Edhouse J, Brady WJ, Morris F. ABC of clinical electrocardiography: Acute myocardial infarction-Part II. BMJ. 2002; 324: 963-6. [full text]
Advanced Reading
Online
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
- Wiesbauer F. Little Black Book of ECG Secrets. Medmastery PDF
Textbooks
- Zimmerman FH. ECG Core Curriculum. 2023
- Mattu A, Berberian J, Brady WJ. Emergency ECGs: Case-Based Review and Interpretations, 2022
- Straus DG, Schocken DD. Marriott’s Practical Electrocardiography 13e, 2021
- Brady WJ, Lipinski MJ et al. Electrocardiogram in Clinical Medicine. 1e, 2020
- Mattu A, Tabas JA, Brady WJ. Electrocardiography in Emergency, Acute, and Critical Care. 2e, 2019
- Hampton J, Adlam D. The ECG Made Practical 7e, 2019
- Kühn P, Lang C, Wiesbauer F. ECG Mastery: The Simplest Way to Learn the ECG. 2015
- Grauer K. ECG Pocket Brain (Expanded) 6e, 2014
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric 6e, 2008
- Chan TC. ECG in Emergency Medicine and Acute Care 1e, 2004
LITFL Further Reading
- ECG Library Basics – Waves, Intervals, Segments and Clinical Interpretation
- ECG A to Z by diagnosis – ECG interpretation in clinical context
- ECG Exigency and Cardiovascular Curveball – ECG Clinical Cases
- 100 ECG Quiz – Self-assessment tool for examination practice
- ECG Reference SITES and BOOKS – the best of the rest
ECG LIBRARY
Emergency Physician in Prehospital and Retrieval Medicine in Sydney, Australia. He has a passion for ECG interpretation and medical education | ECG Library |
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner


really excellent explanation, thanks
great great great explanation…thank you guys
advice against adding fluids in this situation, favoring inhaled nitroglycerin etc
https://emcrit.org/emcrit/right-heart-sara-crager/
https://emcrit.org/pulmcrit/ntg/
https://emcrit.org/emcrit/inhaled-pulmonary-vasodilators/
This is great. I need resources like this since I have been retired for several years and planning on taking a job again in the pre hospital field.
If they’re hypertensive with a inferior omi with confirmed RVI, can be give nitrates or not? I know we need watch as they’re preload sensitive, but what would be best for long pt contact times?
Excellent presentation. Really it will be very much helpful for the students and doctors.
Thanks for the best explanation
Thank you for clarifying the RVMI