R&R In The FASTLANE 021
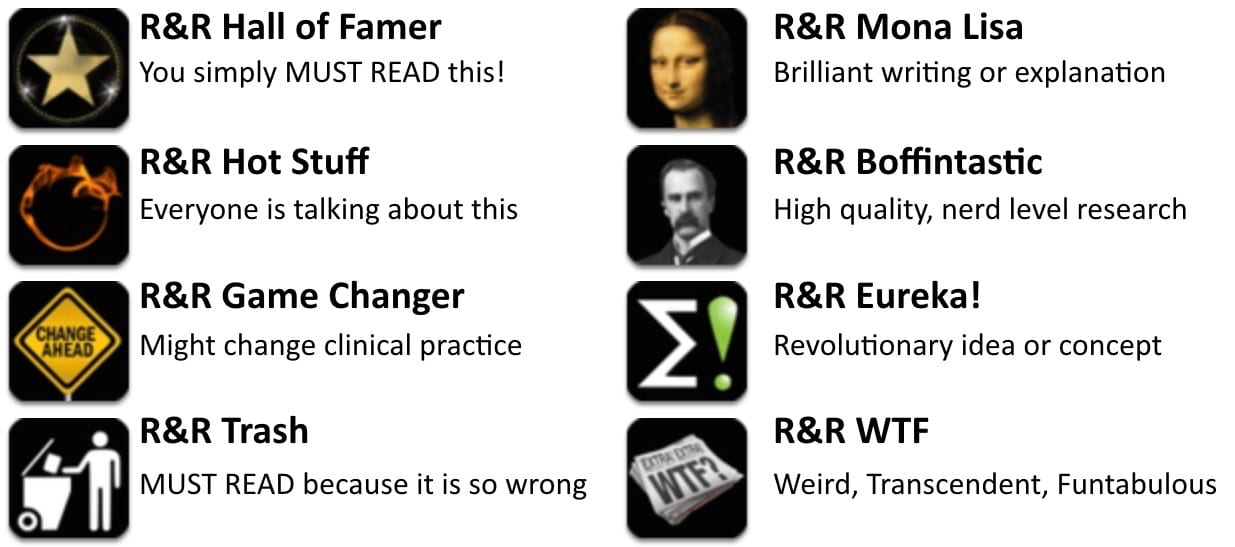
Welcome to the 21st edition of Research and Reviews in the Fastlane. R&R in the Fastlane is a free resource that harnesses the power of social media to allow some of the best and brightest emergency medicine and critical care clinicians from all over the world tell us what they think is worth reading from the published literature.
This edition contains 8 recommended reads. The R&R Editorial Team includes Jeremy Fried, Nudrat Rashid, Soren Rudolph, Anand Swaminathan and, of course, Chris Nickson. Find more R&R in the Fastlane reviews in the : Overview; Archives and Contributors
This Edition’s R&R Hall of Famer
Campagna JD, Bond MC, Schabelman E, Hayes BD. The Use of Cephalosporins in Penicillin-allergic Patients: A Literature Review. J Emerg Med. 2012 May;42(5):612-20. Epub 2011 Jul 13. PMID: 21742459
- It’s probably time to leave 40 year-old data behind and go ahead and use 3rd-generation cephalosporins with impunity in patients with documented penicillin allergies.(RR)
- I have no idea why this old myth needs to be re-killed every couple of years, but people still seem to believe in it. The conclusion that cephalosporins and penicillins have negligible cross reactivity is backed up by decades worth of data.(AB)
- Recommended by Ryan Radecki, Andrew Brainard
- Learn more: EM Literature of Note: Cephalosporins can be used in penicillin allergy
The IST-3 collaborative group. The benefits and harms of intravenous thrombolysis with recombinant tissue plasminogen activator within 6 h of acute ischaemic stroke (the third international stroke trial [IST-3]): a randomised controlled trial. Lancet. 2012 May 23. [Epub ahead of print] PubMed PMID: 22632908
- More stroke data – this time no benefit was demonstrated for the primary outcome. Lots of subgroups, some did better with TPA, some did not. Incredibly rich dataset for us to analyze for the next few years. (RR)
- The study’s conclusions are breathtaking. Not because of the study results, which are unsurprising, but because the authors’ conclusions suggest that they have gone stark, raving mad. (DN)
- Recommended by: Ryan Radecki
- Learn more:
- EM Literature of Note — The Third International Stroke Trial: IST-3
Wilcox SR, Bittner EA, Elmer J, Seigel TA, Nguyen NT, Dhillon A, Eikermann M, Schmidt U. Neuromuscular blocking agent administration for emergent tracheal intubation is associated with decreased prevalence of procedure-related complications. Crit Care Med. 2012 Jun;40(6):1808-1813. PubMed PMID: 22610185.
- I don’t care how many debates Scott Weingart loses, I’m still using neuromuscular blockers for rapid sequence intubation and this new prospective observational study is another reason why.
- Recommended by: Chris Nickson
- Learn more: EMCrit Podcast 061 – Debate: Paralytics for ICU Intubations?
Newman DH. Truth, and epinephrine, at our fingertips: unveiling the pseudoaxioms. Ann Emerg Med. 2007 Oct;50(4):476-7. Epub 2007 Aug 24. PubMed PMID: 17719691 – [Fulltext]
- A great commentary by David Newman on a paper debunking digital ischaemia from adrenaline-containing local anaesthetics. This serves as a call for clinicians, educators, researchers and journals to seek out the pseudoaxioms of medicine and bring about their downfall. Pseudoaxioms are “are false principles or rules often handed down from generation to generation of medical providers and accepted without serious challenge or investigation”.
- Recommended by: Chris Nickson
Puskarich MA, Trzeciak S, Shapiro NI, Arnold RC, Heffner AC, Kline JA, Jones AE; Emergency Medicine Shock Research Network (EMSHOCKNET). Prognostic value and agreement of achieving lactate clearance or central venous oxygen saturation goals during early sepsis resuscitation. Acad Emerg Med. 2012 Mar;19(3):252-8. doi: 10.1111/j.1553-2712.2012.01292.x. PubMed PMID: 22435856; PubMed Central PMCID: PMC3313083.
- More good data from the EMSHOCKNET group – septic patients who cleared lactate but didn’t reach SCVO2 goal did better than if SCVO2 improved but didn’t clear lactate. (This is likely more prognostic than anything, but another it’s another piece in the foundation for noninvasive sepsis management for patients who don’t require pressors.
- Recommended by: Seth Trueger
Wiler JL, Beck D, Asplin BR, Granovsky M, Moorhead J, Pilgrim R, Schuur JD. Episodes of care: is emergency medicine ready? Ann Emerg Med. 2012 May;59(5):351-7. Epub 2011 Sep 29. PubMed PMID: 21963317.
- Discussion of payment models isn’t particularly exciting, but there are a lot of changes under way and if we don’t get paid, we can’t buy new CMAC’s with disposable blade sheaths. There is a push from the current fee-for-service model to “episodes of care” (similar to capitation) and this article explains the basics, the reasoning, and why it may or may not be relevant for emergency care. Payment changes are coming (to the USA), and we need to be ready.
- Recommended by: Seth Trueger
Randolph C. Baseline neuropsychological testing in managing sport-related concussion: does it modify risk? Curr Sports Med Rep. 2011 Jan-Feb;10(1):21-6. Review. PubMed PMID: 21228656.
- Picks apart the validity of the ‘second impact syndrome’ in sports concussion and questions the validity of sideline neuropsychiatric tests like ImPACT, SCAT2 and King-Devick.
- Recommended by: Matthew Mac Partlin
Wright DW, Kellermann AL, Hertzberg VS, Clark PL, Frankel M, Goldstein FC, Salomone JP, Dent LL, Harris OA, Ander DS, Lowery DW, Patel MM, Denson DD, Gordon AB, Wald MM, Gupta S, Hoffman SW, Stein DG. ProTECT: a randomized clinical trial of progesterone for acute traumatic brain injury. Ann Emerg Med. 2007 Apr;49(4):391-402, 402.e1-2. Epub 2006 Sep 29. PubMed PMID: 17011666
- Progesterone for TBI – better evidence than most of what we do now? More studies needed…
- Recommended by: Casey Parker
- Learn more: Cochrane Library — Progresterone for acute brain injury
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC