Sedating Antihistamines
The sedating antihistamines include brompheniramine, chlorpheniramine, cyproheptadine, dexchlorpheniramine, dimenhydrinate, diphenhydramine, doxylamine, pheniramine and promethazine. In overdose they cause dose-dependent CNS depression, anticholinergic effects and in massive overdose cardiovascular toxicity. These drugs are sometimes abused for their anticholinergic properties.
Toxic Mechanism:
Unlike the non-sedating antihistamines they are more lipophilic and cross the blood-brain-barrier easily. They inhibit the peripheral and central H1 receptors and have a higher affinity for muscarinic, alpha adrenergic and serotingeric (5-HT) receptors. Some lower the seizure threshold – unknown mechanisms and in large overdoses there is sodium and potassium cardiac channel blockade which predisposes to dysrhythmias.
Toxicokinetics:
- Good oral absorption
- Peak effect 2 -3 hours
- Lipid soluble
- Large volume of distribution >4 L/kg
- Hepatic metabolism and half lives vary between 6 to 18 hours
Resuscitation:
- Rarely required
- Seizures: (Are rare even though all agents lower the seizure threshold)
- IV benzodiazepines incrementally dosed every 5 minutes to effect.
- Check the patient is not in a dysrhythmia
- Can be managed with benzodiazepines (varying doses in the textbooks, easy method is 0.1mg/kg IV for lorazepam (max 4mg) / midazolam (max 10mg) / diazepam (max 10mg). Or…
- Lorazepam 0.1mg/kg max 4mg
- Diazepam 0.15mg/kg max 10mg
- Midazolam 0.2mg/kg max 10mg
- Hypotension: Usually responds to fluid administration, noradrenaline is second line therapy [0.15mg/kg in 50ml D5W at 1-10ml/hr (0.05 – 0.5 mcg/kg/min)].
- In the rare event of QRS prolongation with ventricular dysrhythmia, treat as per sodium channel blockade. Sodium bicarbonate bolus 1-2 mmol/kg at 3 – 5 minute intervals, once haemodynamically stable, intubate and ventilate to a pH of >7.5
- Torsades de pointes:
- Correct hypoxia, hypokalaemia, hypomagnesaemia and hypocalcaemia
- If the heart rate is < 100 beats/minute consider isoprenaline infusion IV (1 – 10 microgram/minute or 0.05 – 2 microgram/minute in children) or override pacing to maintain a heart rate of 100 – 120 beats/minute
Risk Assessment
- Dose dependent sedation, anticholinergic effects and orthostatic hypotension.
- Large overdoses predispose to prolongation of the QRS and QT intervals leading to cardiac instability requiring inotropes, sodium bicarbonate, intubation and ventilation and correction of electrolytes.
- Children: Ingestion is associated with drowsiness and anticholinergic features.
Supportive Care
- Agitation: Titrated doses of benzodiazepines are effective e.g. diazepam 2.5 – 5 mg every 5 minutes IV until gentle sedation is achieved.
- Check for urinary retention – benzodiazepines will not fix this.
Investigations
- Screening: 12 lead ECG, BSL, Paracetamol level
- Specific:
- If symptomatic patients receive cardiac monitoring for at least 6 hours and a 12 lead ECG every 6 hours until clinical improvement. Once the patient is improving and there is no cardiac abnormality no further ECGs are required.
- The most common situation would be someone who presents and an ECG is done on presentation and at 6 hours which is normal and the patient is asymptomatic, no further ECGs will be required.
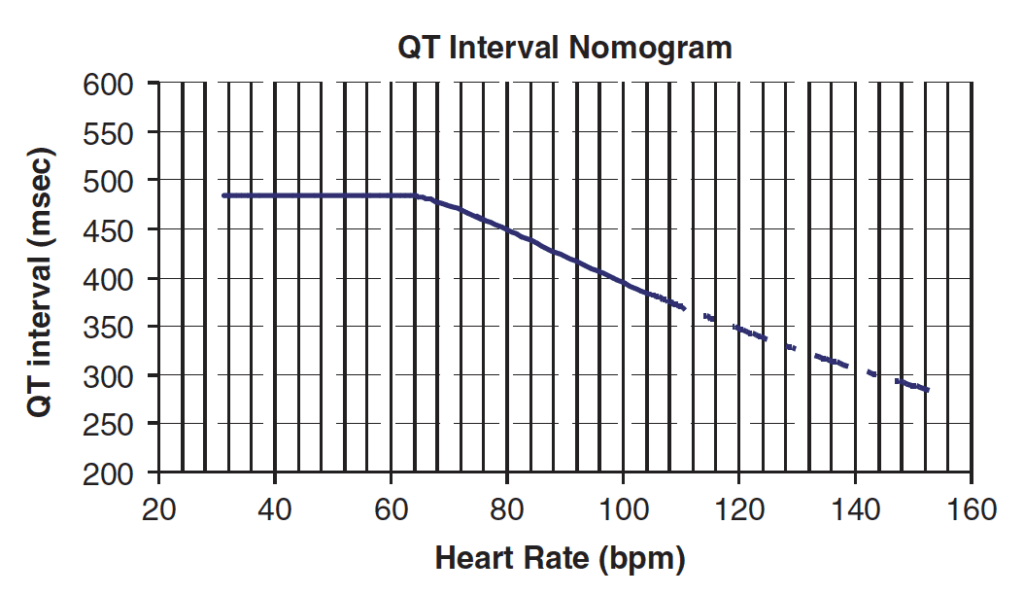
- The QT should be measured on the QT nomogram (not Bazetts formula in toxicology). Technically the average QT of 6 leads should be plotted on the nomogram but recent evidence would indicate lead V2 is the most accurate if only one lead is to be used.
QT Nomogram
Decontamination:
- Not usually indicated as sedation occurs within a couple of hours post ingestions and good outcomes are achieved with supportive care. Anyone intubated should receive activated charcoal via a nasogastric tube 50g (1g/kg in children – max 50g)
Enhanced Elimination
- Not clinically useful.
Antidote
- Physostigmine if anticholinergic delirium is severe.
Disposition
- If patients are asymptomatic at 6 hours post ingestion with a normal 12 lead ECG are medically cleared. Do not discharge overnight.
- Patients with mild anticholinergic features and a normal ECG can be observed on the ward until symptoms resolve and they can ambulate, pass urine and eat and drink.
- Ongoing cardiac monitoring is required for those patients with cardiac abnormalities on their ECGs until it resolves.
- Patients with significant agitation or cardiac dysrhythmias require admission to HDU or ICU
Additional Resources and References
Additional Resources:
- ECG Library – Drugs causing QT prolongation
- Tox Flashcard – Anticholinergic Toxidrome
Sodium Channel Blockade and the ECG
References:
- Burns MJ, Linden CH, Graudins A, et al. A comparison of physostigmine and benzodiazepines for the treatment of anticholinergic poisoning. Annals of Emergency Medicine 2000; 35(4):374-381.
- Clark RF, Vance MV. Massive diphenhydramine poisoning resulting in a wide-complex tachycardia: successful treatment with sodium bicarbonate. Annals of Emergency Medicine 1992; 21:318-321.
- Isbister GK. Risk assessment of drug-induced QT prolongation. Australian Prescriber 2015; 38(1):20-24
- Murray L et al. Toxicology Handbook 3rd Edition. Elsevier Australia 2015. ISBN 9780729542241
- Rotella JA, Taylor DM, Wong A, Greene SL. Accuracy of QT interval measurements on electrocardiographs displayed on electronic ‘smart’ devices. Emergency Medicine Australia 2016; 28:187-192

Toxicology Library
DRUGS and TOXICANTS
Dr Neil Long BMBS FACEM FRCEM FRCPC. Emergency Physician at Kelowna hospital, British Columbia. Loves the misery of alpine climbing and working in austere environments (namely tertiary trauma centres). Supporter of FOAMed, lifelong education and trying to find that elusive peak performance.