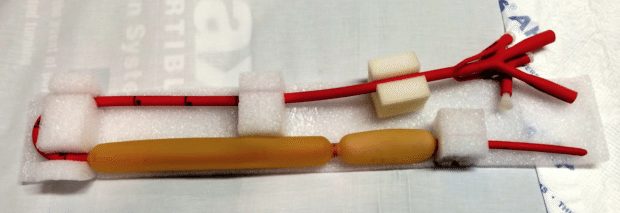
Sengstaken–Blakemore and Minnesota Tubes
OVERVIEW
Sengstaken–Blakemore tube (3 lumen) replaced by Minnesota tube (4 lumen) as allows aspiration of both gastric and oesophageal contents, not just gastric contents
USE
- tamponade of gastro-oesophageal bleeding that is unresponsive to medical and endoscopic treatment (~90% effective)
DESCRIPTION
Sengstaken-Blakemore tube (has ports for gastric and esophageal balloons and a gastric aspiration port)
Minnesota tube (has an esophageal aspiration port in addition to the gastric aspiration port)
METHOD OF INSERTION
- patient is often endotracheally intubated first
- local anaesthetic jelly to nostril
- supine with 45 degrees head up
- estimate length by bridge of nose to xiphoid process
- check both balloons for leaks
- evaluate compliance curve of gastric balloon pre-insertion by inflating the balloon with incremental 100ml aliquots of air to maximal recommended volume (usually 250 -300ml for SBT, 450-500ml for Minnesota) and note the corresponding balloon pressure at each step
- lubricate balloons
- insert via mouth via laryngoscopy into the oesophagus
- confirm position on CXR (gastric balloon in stomach)
- inflate gastric balloon using 50mL increments up to 250 -300ml for SBT or 450-500ml for Minnesota tube
- If, post-insertion, balloon pressure on inflation with a given volume is >15 mmHg than the pre-insertion pressure, the balloon may be in the oesophagus and should be deflated and position checked
- pull balloon back until against gastric fundus
- note measurement at lips and fix securely with traction and rope pulley system with 500mL bag of fluid
- inflation of oesophageal balloon usually is not required (if required inflate to 40mmHg)
- never use on its own
- use only if continuing bleeding despite an adequately inflated gastric balloon correctly placed and with appropriate tension
OTHER INFORMATION
- avoid inflation of gastric balloon in oesophagus as this is almost always fatal!
- CXR prior to balloon inflation and after inflation or fluoroscopic insertion
COMPLICATIONS
- haemorrhage (note that re-bleeding on balloon deflation occurs in ~50% of cases)
(check position, ensure balloon inflated, correct coagulopathy) - painful or uncomfortable
(check position; provide sedation and analgesia) - aspiration
(use only in intubated patient and position patient head-up 30-45 degrees) - pressure necrosis
(do not leave SBT in situ for more than 24-36 h, avoid prolonged inflation of gastric balloon – deflate after 12 hr and reinflate if ongoing bleeding) - oesophageal perforation
(ensure both balloons completely deflated prior to insertion, avoid inflation of oesophageal balloon, and ensure gastric balloon is correctly positioned during inflation) - acute upper airway obstruction due to balloon migration
(avoid use in unintubated patient — if SBT in unintubated patient and develops respiratory distress, immediately cut lumens for oesophageal and gastric balloons and remove tube) - cardiac arrhythmias
(check position; correct electrolytes; cardioversion)
VIDEO
References and Links
FOAM and web resources
- EMCrit — Blakemore Tube Placement for Massive Upper GI Hemorrhage (2013)
- EMCrit — PulmCrit Wee: Ultrasound-guided blakemore tube placement (2016)
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC

