Sepsis Literature Summaries
ANTIBIOTICS
Kumar, A et al Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006 Jun;34(6):1589-96. PMID 16625125
- retrospective co-hort study
- aim = to study the impact of delays and of appropriate antimicrobial therapy on mortality in patients presenting with septic shock
- n = 2731 with shock (558 received A/B pre-shock, 19 no shock)
- inclusion criteria: adult, septic shock
- exclusion criteria: A/B before shock, no A/B
- 14 ICU’s in USA and Canada
- looked at: (1) time of onset of septic shock, (2) time of onset of antibiotics.
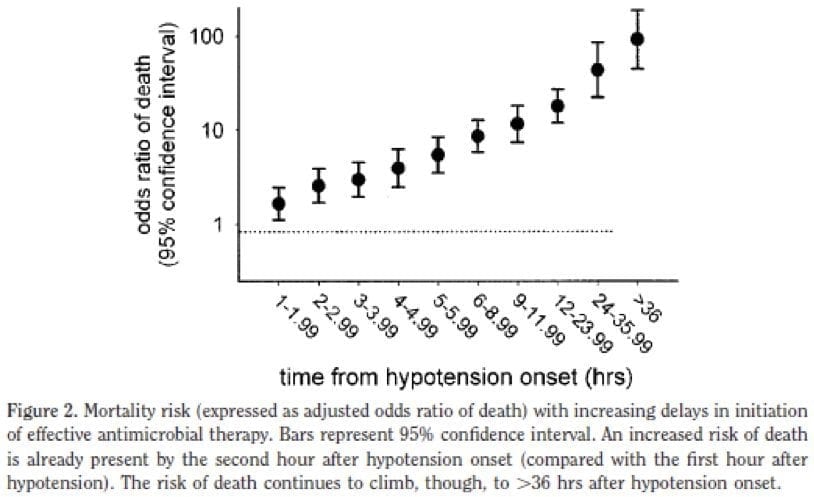
- strong relationship between the delay in effective antimicrobial initiation and in-hospital mortality was noted (adjusted odds ratio 1.119 [per hour delay], 95% confidence interval 1.103–1.136, p <.0001).
- average time to antibiotics in the shocked patient was 6 hours.
-> for every hour a patient does not receive appropriate antibiotic therapy there mortality rate increases by 7.5%.
-> if patient receives antibiotics within 1 hour of onset of hypotension -> their in hospital survival = 80%
-> IV access in, blood out (including cultures), A/B in.
INOTROPES/PRESSORS IN SEPSIS
Choong, K., et al. Vasopressin in pediatric vasodilatory shock: a multicenter randomized controlled trial. Am J Respir Crit Care Med. 2009 Oct 1;180(7):632-9 PMID 19608718
- aim = to examine the efficacy and safety of vasopressin in addition to vasoactive agents in the treatment o vasodilatory shock in children
- RCT, double blinded, placebo controlled trial
- inclusion criteria: < 18 years, shock for 24 hours, going to survive > 24 hours
- vasopressin vs normal saline
- primary outcome = time to vasoactive-free haemodynamic stability
- secondary outcomes = mortality, number of days free of organ failure, vasoactive drugs, mechanical ventilation during 30 days after randomized, MAP after study drug infusion, length of critical care unit stay, adverse events
- n = 69
-> no difference with regard to vasoactive free haemodynamic stability
-> no difference in all secondary outcomes
-> thus can’t be recommended in paediatric patients
CAT Study Investigators A comparison of epinephrine and norepinephrine in critically ill patients. Intensive Care Med. 2008 Dec;34(12):2226-34 PMID 18654759
- MRCT
- adrenaline vs noradrenaline for hypotension in ICU
- septic shock and acute circulatory failure patients
- n = 280
- Adrenaline -> transient lactic acidosis, tachycardia, hyperglycaemia
-> no difference shock duration, ventilation, ICU LOS
Annane, D et al. Norepinephrine plus dobutamine vs epinephrine alone for management of septic shock: a randomized trial. Lancet. 2007 Aug 25;370(9588):676-84. PMID 17720019
- MRCT
- adrenaline vs noradrenaline for hemodynamic support
- n = 330 pts with septic shock
-> no difference, mortality. blood pressure, time to hemodynamic stability, duration of vasopressor therapy, time to resolution of organ dysfunction, similar adverse events
EGDT
Jones, A. et al. Lactate Clearance vs Central Venous Oxygen Saturation as Goals of Early Sepsis Therapy: A Randomized Clinical Trial. JAMA. 2010 Feb 24;303(8):739-46. PMID 20179283
Goal = to compare lactate clearance as non-inferior to ScVO2 as a resuscitation target in severe sepsis.
- MRCT
- prospective, randomized, parallel group, non-blinded
- January 2007 – 2009
- 3 US urban hospitals
Inclusion criteria:
- severe sepsis or septic shock admitted to ED
- > 17 years
- confirmed or presumed infection
- 2 or more SIRS criteria
- hypoperfusion (SBP < 90mmHg post 20mL/kg volume or a blood lactate of at least 4.0mmol/L
- Exclusion criteria:
– pregnancy
– primary diagnosis other than sepsis
– suspected requirement for immediate surgery within 6 hours of diagnosis
– an absolute contraindication to check or neck CVL
– CPR
– transfer from another institution with a sepsis-specific resuscitative therapy underway
– advanced directive orders that would restrict the study procedure - Results:
-> ScvO2 group mortality rate = 23%
-> lactate clearance group mortality rate = 17%
-> patients with septic shock and resuscitated to a normal CVP and MAP when randomised to target SvO2 vs lactate clearance of 10% -> there was no difference in mortality.
-> lactate measurements in peripheral venous blood is as safe and efficacious as a computerised spectrophotometric catheter in sepsis resuscitation.
Rivers. Early goal-directed therapy in the treatment of Severe Sepsis and Septic Shock” NEJM 2001; 345: 1368-1377
- RCT
- standard care vs 6 hours of targeted resuscitation (MAP > 65, CVP 8-12, ScvO2 > 70%, U/O > 0.5-1mL/kg, HCT > 30%, lactate, pH, BE)
- treatment group received more fluid, inotropes and RBC’s
-> mortality reduction = 15%
-> NNT to prevent death = 6-8 - criticisms: single centre, high mortality in control group (46%), treatment group resuscitated by Rivers!, Rivers worked for Edwards Life Sciences, very aggressive and invasive -> multiple interventions tested at the same time
ARISE Trial
- ANZICS trial
- MRCT
- early goal directed therapy vs conventional care (testing the data from single centre Rivers trial)
CATHETER RELATED BLOOD STREAM INFECTIONS
Darouiche R.O, et al. Catheter Study Group. A comparison of two anti-microbial-impregnated central venous catheters. NEJM 1999; 340: 1-8
- RCT
- inclusion: requires a CVL for atleast 3 days
- antibiotic impregnanted CVL: minocycline + rifampicin VS chlorhexidine + silver sulfadiazine
- n = 865
-> significant reduction in rates of colonisation and CRBI in antibiotic impregnated group
Veenstra DL. et al. Efficacy of antiseptic-impregnated central venous catheters in preventing catheter-related blood stream infections: a meta-analysis. JAMA. 1999 Jan 20;281(3):261-7. PMID 9918482
- -> chlorhexidine + silver sulfadiazine catheters have been shown to be superior to standard lines
Pronovost, P. et al. An Intervention to Decrease Catheter-Related Bloodstream Infections in ICU. NEJM 2006; 355:(26): 2725-32 PMID 17192537
- prospective co-hort study
- goal = implementation of 5 evidence based guidelines to decrease the incidence of catheter-related blood stream infections
- interventions: hand washing, full barrier precautions, chlorhexidine, avoid femoral site, remove unnecessary catheters early
- primary outcome = rate of infections reduced during first 3 months of implementation
- secondary outcome = decrease rate would be sustained.
- 108 ICU’s involved
- 375,757 catheter days
-> primary and secondary outcomes accomplished with statistical significance
Chaiyaku-napruk, N. et al (2002) Ann Intern Med 136:792-801
- meta-analysis
-> use alcohol 75% + chlorhexidine 1%
Lane, R.K et al. Central Line Infections. Current Opinion Crit Care 2002; 8: 441-448
- don’t routinely change lines
- SC better than IJ better than femoral
- changing lines over a guidewire increases colonisation but not catheter related blood stream infection
Summary
- antibiotics better than anti-septic better than standard
- SC better than IJ better than femoral
- use chlorhexidine 1% + alcohol 75% over povidone-iodine
- don’t routinely change lines (change for fever)
- changing lines over a guidewire increases colonisation but not catheter related blood stream infection
ACTIVATED PROTEIN C
- in sepsis there are documented low levels of APC -> associated with increased negative outcomes (increased shock and mortality)
- improves neutrophil and endothelial interaction -> improves microvascular patency
PROWESS
- MRCT (2001, NEJM)
- n = 1690
- APC vs Placebo in SIRS + atleast one organ dysfunction
-> 6% mortality reduction (more apparent in sicker patients)
-> no significant rise in bleeding
ENHANCE
- Multicenter (2005, CCM) – single arm open label
- n = 2378
-> similar mortality rates to PROWESS
-> increased bleeding (ICH)
ADDRESS
- MRCT (2005, NEJM) – 516 Centers, 34 Countries
- n = 1610
- Goal = quantify risk of bleeding in those @ low risk of death
-> serious bleeding: 4% in APC and 2% in Placebo
-> no role of APC in those at low risk of death
PROWESS SHOCK
- TBC
MISCELLANEOUS
de Gans, J et al – European Dexamethasone in Adulthood Bacterial Meningitis Study Investigators (2002) “Dexamethasone in adults with bacterial meningitis” NEJM 347:1549-1556
- MRCT
- n = 301
- dexamethasone 10mg 20min prior or with first dose of antibiotics -> Q6 hrly for 4 days VS placebo
- 65% were Streptococcus pneumoniae and Neisseria meningitidis
-> reduced mortality in Pneumococcus
-> improved score on Glasgow Outcome Scale
-> no difference in hearing or focal neurological signs
Dellinger, R.P. et al (2004) “Surviving sepsis campaign guidelines for management of severe sepsis and septic shock” Critical Care Medicine 32:585-873
- evidence based recommendations for the management of sepsis with intention to improve outcomes
- come conclusions are hotly debated
Lee, W et al (2010) “Sepsis and Endothelial Permeability” New England Journal of Medicine, 363:7 page 689
- endothelial permeability = major problem in sepsis
-> important mediator in the maintenance of endothelial integrity found – Slit protein -> Robo4 receptor -> prevent dissociation of p120-catenin and VE-cadherin in response to inflammatory mediators in animal models -> shown to significantly decrease mortality in animal models using different sepsis models.

Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC