Serotonin toxicity
aka Toxicology Conundrum 024
A 23 year-old female is brought to your ED by a friend. She appears anxious, distressed and confused. Her vital signs are:
- T 37.4C
- P 110/min
- RR 19/min
- BP 160/100 mmHg
- SO2 98% OA
- GCS 13 (E4V3M6)
The patient is unable to give a coherent history. Her friend volunteers that the patient had seen a GP in the past few weeks as she was feeling depressed. The friend also admitted that the patient occasionally used recreational drugs such as marijuana and ecstasy.
Further of examination of the patient was notable for the presence of shaking eye movements, brisk deep tendon reflexes, sustained clonus and stiffness of the lower limbs.
Before answering the questions – do you remember this from Toxicology Conundrum 017?
Questions
Q1. What is the likely diagnosis?
Answer and interpretation
- Serotonin toxicity, aka serotonin syndrome
Q2. Describe the clinical manifestations of this condition?
Answer and interpretation
Serotonin syndrome typical resolves within 12 -24 hours. Exceptions may occur following massive overdoses, in the presence of multiple serotonergic agents (especially MAOIs) and in the context of intercurrent illness.
Serotonin syndrome has 3 types of clinical manifestations (‘CAN’):
- central nervous system
- altered mental state (agitation, anxiety, confusion or stupor), seizures
- autonomic dysfunction
- hypertension or hypotension, tachycardia or bradycardia, hyperthermia, dysrhythmias, flushing, sweating, mydriasis
- neuromuscular dysfunction
- rigidity (lower limbs more so than upper limbs), hyper-reflexia, clonus (including ocular), tremor, myoclonus
Q3. How is this diagnosis made?
Answer and interpretation
Serotonin toxicity can be diagnosed using the Hunter Serotonin Toxicity Criteria.
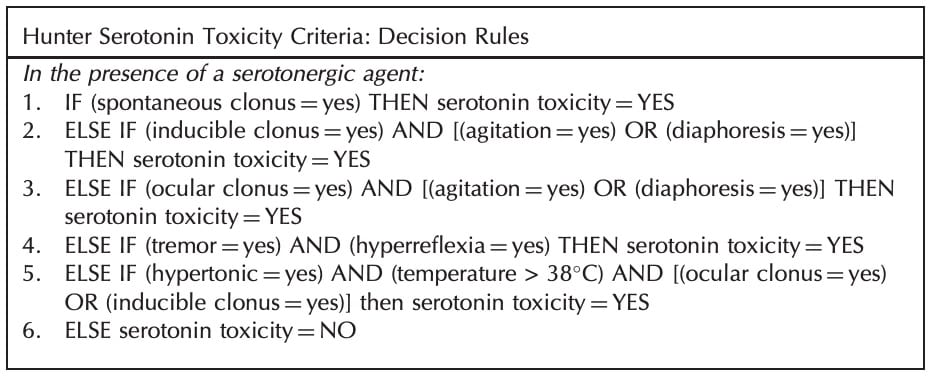
- use of a serotonergic agent in the past 5 weeks,
- AND
- no other cause present,
- AND
- spontaneous clonus,
- OR
- tremor and hyperthermia,
- OR
- inducible OR ocular clonus, AND either of:
- diaphoresis OR agitation,
- OR
- rigidity AND hyperthermia.

The Hunter Serotonin Toxicity Criteria – believe it or not – are simpler than the original Sternbach criteria for diagnosing serotonin syndrome and are more sensitive (84%) and more specific (97%).

In practice, the diagnosis is often more of a gestalt impression based of the history, absence of other causes and the findings on physical examination.
Q4. What are the main differential diagnoses?
Answer and interpretation
The differential diagnosis of serotonin syndrome is extensive.
Drugs, poisons and toxins
- anticholinergic syndrome
- neuroleptic malignant syndrome
- sympathomimetic syndromes
- salicylism
- theophyline toxicity
- nicotinic toxicity
Encephalopathies
- metabolic
- infective
- organic brain disorders
Psychiatric disorders
- including lethal catatonia
Malignant hyperthermia
Q5. What are the potential underlying causes?
Answer and interpretation
Serotonergic agents are the cause – funnily enough – either in overdose or a combination of therapeutic agents. Here are the main groups with common examples:
- Selective-serotonin reuptake inhibitors (SSRIs)
- [fluoxetine, paroxetine, citalopram.]
- Selective noradrenergic reuptake inhibitors (SNRIs)
- [duloxetine, reboxetine (not so selective in overdose or in combination with others!)]
- Opioids and related drugs
- [pethidine, fentanyl, tramadol, dextromethorphan.]
- Tricyclic antidepressants (TCAs)
- [amitryptyline, nortriptyline, dothiepin.]
- monamine oxidase inhibitors (MAOIs)
- [moclobemide, tranylcypramine.]
- Antibiotics
- [linezolid]
- Antiemetics
- [metoclopramide, ondansetron.]
- Mood stabilisers
- [lithium, sodium valproate.]
- Recreational drugs
- [amphetamines, ecstasy, lysergic acid (LSD)]
- Herbal agents
- [St. John’s Wort, Ginseng.]
Q6. What investigations are indicated?
Answer and interpretation
Usually of greater importance than investigations is obtaining a reliable history of exposure to serotonergic agents. This should be vigorously pursued:
- call GP and/or pharmacist
- check scripts
- ask paramedics if they searched the scene – consider arranging a ‘House, MD’ style investigation of the scene…
- talk to family and friends regarding access to, and use of, pharmaceuticals, recreational drugs or herbal remedies
Investigations:
- screening tests – ethanol level, APAP level, ECG, BSL.
- check for complications and rule out other differential diagnoses – CK, urinalysis (including myoglobin), UEC, ABG as required.
Q7. When would you consider intubating and ventilating this patient?
Answer and interpretation
Intubation may be indicated for airway protection:
- decreased GCS is associated with increased aspiration risk
— GCS<12 is a somewhat arbitrary threshold; GCS 8 has not been validated in toxicological settings - prolonged or recurrent seizures
Intubation, ventilation and paralysis may be indicated for severe serotonin syndrome independent of the need for airway protection:
- truncal rigidity impeding ventilation
- hyperthermia (T39.5C+)
- rising PaCO2
- rising CK
Q8. Describe your management plan for this patient?
Answer and interpretation
As always, using the ‘Resus-RSI-DEAD’ approach:
Resuscitation —
- Assess the patient in a setting suitably staffed and equiped for resuscitation and monitoring.
- Identify immediate life threats:
— decreased level of consciousness
— rigidity, hyperthermia and hypercapnea: requires intubation, ventilation and neuromuscular blockade
— seizures - Airway, Breathing, Circulation:
— administer oxygen
— check cardiac rhythm and output
— establish IV access - Check for and correct hypoglycaemia:
— if glucose <4mM then administer 50mL of 50% dextrose IV (5ml/kg of 10% dextrose in children) - Control ongoing seizures (see Toxicology Conundrum #023):
- benzodiazepines are first line:
e.g. diazepam 5-10mg IV over 3-5 min (0.1-0.3 mg/kg in children) repeated as necessary. - barbiturates are second line:
e.g. phenobarbitone 100-300mg slow IV (10-20 mg/kg in children) or thiopentone IV 3-5 mg/kg (if intubated and ventilated) - refractory seizures require intubation and ventilation with continuous sedation.
- benzodiazepines are first line:
- Correct hyperthermia:
— continuously monitor if T>38.5 C
— consider intubation and ventilation with neuromuscular blockade if T >39.5 C - Discontinue any sertonergic agents and avoid administration of further serotonergic agents.
Risk assessment —
- this patient has serotonin syndrome probably due to a combination of antidepressants and recreational drugs. It is likely to resolve over 1-2 days. More history is needed regarding drugs ingested, doses, times of ingestion and comorbidities.
Supportive care and monitoring —
- reassurance and careful observation
- fluid management
- agitation, hypertension and tachycardia – usually responds to benzodiazepines
- consider the potential for rhabdomyolysis – see Laboratory Tester #002 for management.
Investigations — see Q6 above.
Decontamination —
- activated charcoal (50g PO/NG) should only be administered if the airway is secure and will remain so (e.g. post intubation).
Enhanced Elimination — nil.
Antidotes —
- Benzodiazepines are the mainstay of treatment as noted above.
- Serotonin antagonists are of unproven efficacy and may have side-effects
- cyproheptadine
— consider if prolonged or benzodiazepine-resistant
— 12mg NG, if clinical response noted administer 8mg q8h for 24h - olanzapine — 10mg SL
- chlorpromazine — 25-100mg in 100 mL normal saline over 30-60 minutes
- cyproheptadine
Disposition —
- very mild cases may be discharged with symptomatic treatment, reassurance and appropriate follow up (e.g. GP or mental health team).
- patients with abnormal mental state or vital signs require admission (usually for about 24h) for observation, supportive care and pharmacotherapy until symptoms resolve.
- severe cases require ICU level care (e.g. intubation and ventilation).
- patients at risk of serotonin syndrome due to a deliberate self-poisoning should be observed for at least 8 hours and not discharged at night. This may vary depending on the risk assessment of the specific agent ingested.
Q9. What are the 5 clinical settings when this diagnosis should be suspected?
Answer and interpretation
Serotonin toxicity typically occurs in one of these settings:
- overdose of a serotonergic agent
- initation or increase in dose of a serotonergic agent
- replacement of one serotonergic agent with another, without an adequate washout period
- interaction of 2 or more therapeutic agents
- interaction of a therapeutic agent with a recreational drug or an alternative medicine.
References
- Sternbach H. The serotonin syndrome. Am J Psychiatry. 1991 Jun;148(6):705-13.
- Dunkley EJ, Isbister GK, Sibbritt D, Dawson AH, Whyte IM. The Hunter Serotonin Toxicity Criteria: simple and accurate diagnostic decision rules for serotonin toxicity. QJM. 2003 Sep;96(9):635-42
- Boyer EW, Shannon M. The serotonin syndrome. The New England journal of medicine, 2005;352 (11), 1112-20
- Isbister GK, Buckley NA, Whyte IM. Serotonin toxicity: a practical approach to diagnosis and treatment. Med J Aust. 2007 Sep 17;187(6):361-5.
- Torre LE, Menon R, Power BM. Prolonged serotonin toxicity with proserotonergic drugs in the intensive care unit. Crit Care Resusc. 2009 Dec;11(4):272-5

CLINICAL CASES
Toxicology Conundrum
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
