Stevens-Johnson syndrome
Description
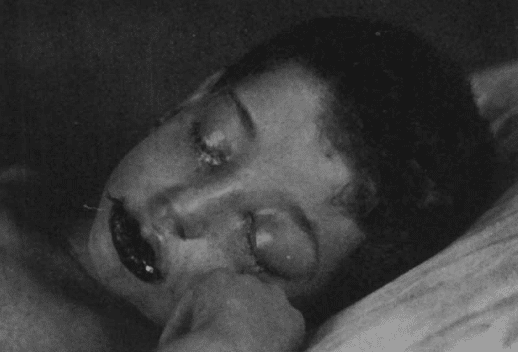
Stevens-Johnson syndrome is an immunological skin conditions, often secondary to drugs or infection. Initial presentation is usually a feverish prodromal period followed by a blistering erythematous skin condition – characterised by mucous membrane involvement
History
1844 – Ferdinand Ritter von Hebra (1816-1880) [Translated archive text] Hebra separated from the ill defined group of erythemas an entity which he called “erythema multiforme exudativum.” – a febrile erythema occasionally involving mucous membranes
1855 – Wharton Jones
1922 – Albert Mason Stevens (1884-1945) and Frank Chambliss Johnson (1894-1934) published the case reports of two boys aged 7 and 8 at Bellevue hospital, New York. This report was also published later that year in the Lancet. “A New Eruptive Fever Associated with Stomatitis and Ophthalmia” in children. They could find no description of a similar cutaneous eruption and thought that no known diagnosis could be made from the symptoms and course of the disease.
Two cases have been observed of a generalized cutaneous eruption, not conforming to any recognized dermatologie condition. Both cases occurred in boys, one aged 7, the other 8, coming from widely separated parts of New York City, with no possibility of contact. Both cases manifested a purulent conjunctivitis, in Case 2 going on to panophthalmitis and total loss of vision, and in Case 1 responding to treatment, but leaving a severe corneal scar. The pus showed pyogenic organisms only; no gonococci.
Stevens and Johnson. 1922

Stevens and Johnson were the first to draw attention to the conjunctival involvement of the syndrome which was the distinguishing feature at that time
1929 – CM Rutherford
1930 – John M Wheeler
To two cases previously reported by Stevens and Johnson, and one of probably similar nature reported by Rutherford, the author adds a new case. The condition is febrile, with a general skin eruption not corresponding to any exanthematous or cutaneous disease previously identified. The disease is serious only as regards the eyes, but the incidental membranous conjunctivitis seems to tend to more or less complete destruction of sight, by the development of extremely severe corneal ulceration.
Wheeler 1929
1935 – George J. Ginandes (1904-1988) presented a case, reviewed the literature and suggested the term atypical erythema exudativum multiforme (Stevens-Johnson).
1946 – The Commission on Acute Respiratory Diseases (1946) considered that “The term ‘Stevens-Johnson’ has been applied with increasing frequency in this country although it has no historical justification”
The Commission published six cases of severe erythema multiforme with evidence of a pulmonary involvement in three, and recognized as a non-bacterial pneumonia. The chief purpose of the report was to emphasize the relationship of pneumonia to erythema exudativum multiforme, since lung involvement was a feature not stressed enough in previous descriptions.
1950 – The condition of Stevens-Johnson seemed to be more severe than Hebra. Later authors dividing erythema exudativum multiforme into major (Stevens-Johnson) and minor (Hebra) types
Associated Persons
- Ferdinand Hebra (1816 – 1880)
- Albert Mason Stevens (1884 – 1945)
- Frank Chambliss Johnson (1894 – 1934)
- George J. Ginandes (1904 – 1988)
Alternative names
- There is overlap in the presentation with Toxic Epidermal Necrolysis and erythema multifome exsudativum majus.
- They are all on the spectrum of the same pathogenetic disease process
- Erythema exudativum multiforme (Hebra disease)
References
Original articles
- Hebra F. On diseases of the skin, including the exanthemata. 1866
- Wharton Jones T. Inflammation of the conjunctiva. In; The principles and practice of ophthalmic medicine and surgery. 1855: 61
- Stevens AM, Johnson FC. A new eruptive fever associated with stomatitis and ophthalmia: report of two cases in children. Am J Dis Child. 1922; 24(6): 526-533.
- Stevens AM, Johnson FC. A New Eruptive Fever. The Lancet. 1922; 200(5183): 1396
- Rutherford CW. Membranous Conjunctivitis with Loss of Eyeballs: Report of Cases. JAMA. 1929; 93(23):1779-1784
Reference articles
- Wheeler JM. Destructive Purulent Ophthalmia Accompanying an Eruptive Fever with Stomatitis, American journal of ophthalmology. 1930; 13(6): 508.
- Bailey JH. 1931. Lesion of The Cornea and Conjunctiva in Erythema Exudativum Multifome (Hebra). Arch Ophthalmol. 1931;6(3):362-379.
- Ginandes GJ. Eruptive Fever With Stomatitis and Ophthalmia: Atypical Erythema Exudativum Multiforme (Stevens-Johnson). Am J Dis Child. 1935; 49(5): 1148-1160.
- Fort Bragg NC. Association of pneumonia with Erythema Exudativum Multifome: Commission on Acute Respiratory Diseases. Arch Intern Med (Chic). 1946; 78(6): 687-710.
- Thomas BA. So-called Stevens—Johnson Syndrome. Br Med J. 1950; 1(4667): 1393–1397.
- Bastuji-Garin S et al. Clinical classification of cases of toxic epidermal necrolysis, Stevens-Johnson syndrome, and erythema multiforme. Arch Dermatol. 1993 Jan;129(1):92-6.
- Rzany B et al. Epidemiology of erythema exsudativum multiforme majus, Stevens-Johnson syndrome, and toxic epidermal necrolysis in Germany (1990-1992): structure and results of a population-based registry. J Clin Epidemiol. 1996; 49(7): 769-73.
- Mockenhaupt M. The current understanding of Stevens-Johnson syndrome and toxic epidermal necrolysis. Expert Rev Clin Immunol. 2011; 7(6): 803-13; quiz 814-5.
- Bohigian, George M. The history of Stevens-Johnson Syndrome and a case study. St. Louis: Center for History of Medicine at Washington University School of Medicine, 2015
[cite]
eponymictionary
the names behind the name
BSc, MD from University of Western Australia. Junior Doctor currently working at Sir Charles Gairdner Hospital.

