Sudden Syncope at Soccer
aka ECG Exigency 008
A 26-year old man presents to ED by ambulance after an episode of syncope while playing soccer. On arrival, he is dizzy and slightly pale with a BP of 85/60.
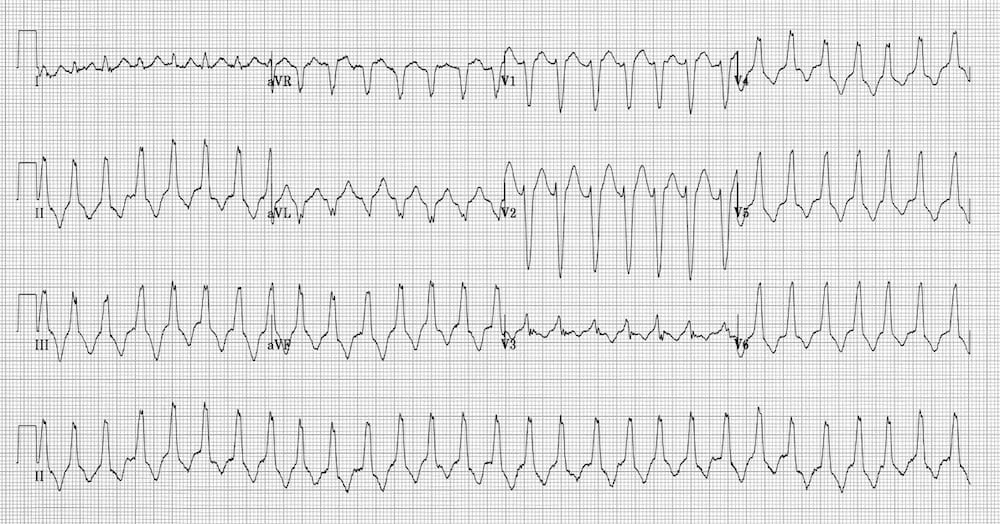
ECG 1 on arrival:
ECG 2 is being taken as the patient becomes unconscious on the trolley

Two cycles of CPR and 100 joules of (biphasic) electricity later, he wakes up with a start and pushes the resuscitating team off his chest.
ECG 3 Post CPR

Questions
Q1. Describe and interpret ECG 1
Answer and Interpretation
The first ECG shows:
- Regular, broad complex tachycardia at around 180 bpm
- Inferior axis (just leftward of +90 degrees)
- LBBB-like morphology to the QRS complexes (dominant S wave in V1)
- No discernible P waves
This is an example of Right Ventricular Outflow Tract Tachycardia (RVOT)
Right Ventricular Outflow Tract Tachycardia (RVOT)
- RVOT is a cyclic-AMP-mediated form of VT that is classically triggered by exercise or catecholamine excess.
- The LBBB morphology and inferior axis are typical of this type of VT.
Two conditions produce RVOT:
- Idiopathic RVOT is a fairly benign condition, more common in young females, that causes recurrent episodes of VT with a LBBB morphology. Patients have structurally normal hearts and the VT usually responds to treatment with beta-blockers.
- The other condition associated with RVOT will be discussed below…
Other differential diagnoses to consider with ECG 1 are:
- SVT with LBBB
- SVT with WPW
Here are some handy tips for differentiating VT from SVT with aberrancy.
Q2. Describe ECG 2
Answer and Interpretation
The second ECG shows:
- Ventricular fibrillation (VF).
NOTE: VF should (hopefully) never be diagnosed from the 12-lead ECG!
Q3. Describe ECG 3
Answer and Interpretation
The third ECG shows:
- Sinus rhythm at around 75 bpm
- Right axis deviation
- Dominant R wave in V1
- T wave inversion in the anterior (V1-6) and inferior (I, II, aVL) leads
- Subtle widening of the QRS complexes in V2-3
- Epsilon waves (a small ‘blip’ after the QRS complex), visible in multiple leads
Q4. What is the diagnosis?
Answer and Interpretation
Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC)
- The combination of a RVOT leading to VF arrest with a resting ECG showing Epsilon waves and signs of right ventricular hypertrophy (T-wave inversion in the right- to mid-precordial leads, dominant R wave in V1, right axis deviation) is diagnostic of ARVC (aka arrhythmogenic right ventricular dysplasia (ARVD))
- An inherited myocardial disease associated with paroxysmal ventricular arrhythmias and sudden cardiac death.
- >Characterized pathologically by fibro-fatty replacement of the right ventricular myocardium.
- The second most common cause of sudden cardiac death in young people (after HOCM), causing up to 20% of sudden cardiac deaths in patients < 35 yrs of age.
- Typically inherited as an autosomal dominant trait, with variable penetrance and expression (there is an autosomal recessive form called Naxos Disease, which is associated with woolly hair and skin changes).
- More common in men than women (3:1) and in people of Italian or Greek descent.
- Estimated to affect approximately 1 in 5,000 people overall.
Diagnosis of ARVD / ARVC
There is no single diagnostic test for ARVD. The diagnosis is made using a combination of clinical, electrocardiographic and radiological features, as defined by the (horribly complicated) 2010 Task Force Criteria.
Clinical Features
- ARVD causes symptoms due to ventricular ectopic beats or sustained ventricular tachycardia (with LBBB morphology) and typically presents with palpitations, syncope or cardiac arrest precipitated by exercise.
- The first presenting symptom may be sudden cardiac death.
- Over time, surviving patients also develop features of right ventricular failure, which may progress to severe biventricular failure and dilated cardiomyopathy.
- There is usually a family history of sudden cardiac death.
ECG Features
ARVD is associated with characteristic ECG abnormalities:
- Epsilon wave (most specific finding, seen in 30% of patients)
- T wave inversions in V1-3 (85% of patients)
- Prolonged S-wave upstroke of 55ms in V1-3 (95% of patients)
- Localised QRS widening of 110ms in V1-3
- Paroxysmal episodes of ventricular tachycardia with a LBBB morphology
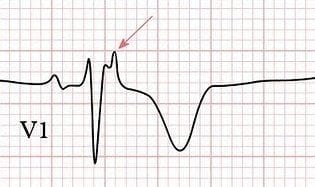

Some authors recommend recording ECG rhythm strips at double speed and double amplitude to enhance the detection of some of these features (click here for a description of how to do this).
Imaging
- Echocardiography is the first-line investigation, and may demonstrate a dilated, hypokinetic right ventricle with prominent apical trabeculae and dilatation of the RV outflow tract.
- The imaging modality of choice in many centres is cardiovascular MRI, which can accurately demonstrate structural and functional features of ARVD such as fibrofatty infiltration and thinning of the RV myocardium, RV aneurysms, RV dilatation, regional wall motion abnormalities and global systolic dysfunction.
- Other imaging modalities such as CT scanning and right ventricular contrast angiographymay be used to make the diagnosis where MRI is unavailable, but have the disadvantages of high radiation burden and/or invasive technique.
- Histological diagnosis, either via endomyocardial biopsy or at autopsy, provides a definitive diagnosis but is impractical, and for those patients diagnosed at post-mortem… far too late!
Risk Assessment
Patients with ARVD are considered to be at high risk of sudden death if they have any of the following:
- A history of syncope due to cardiac arrest
- Recurrent arrhythmias not suppressed by anti-arrhythmic drug therapy
- A family history of cardiac arrest in first degree relatives
Treatment Options
- In patients with no high risk features, initial treatment is with anti-arrhythmic drugs such as beta-blockers or amiodarone to suppress cathecholamine-triggered ventricular arrhythmias. Currently, the most effective drug for this is sotalol.
- Patients with any high risk features require urgent insertion of an implantable cardioverter-defibrillator (ICD).
- In patients with persistent symptomatic arrhythmias, radiofrequency ablation of conduction pathways may be attempted.
- Heart failure is treated in the usual way, with diuretics, ACE inhibitors and anticoagulants. In severe cases, cardiac transplantation may be required.
References
- Protonotarios N, Tsatsopoulou A. Naxos disease. Indian Pacing Electrophysiol J. 2005 Apr 1;5(2):76-80.
- Perez Diez D, Brugada J. Diagnosis and Management of Arrhythmogenic Right Ventricular Dysplasia European Society of Cardiology 2008
- Kottkamp H, Hindricks G. Right ventricular tachycardia-arrhythmogenic right ventricular cardiomyopathy or idiopathic? Eur Heart J. 2003 May;24(9):787-8.
- Corrado D, Biffi A, Basso C, Pelliccia A, Thiene G. Twelve-lead ECG in the athlete: physiological versus pathological abnormalities. Br J Sports Med 2009; 43:669-676. [PMID: 19734501]
- Anderson EL. Arrhythmogenic right ventricular dysplasia. Am Fam Physician. 2006 Apr 15;73(8):1391-8 [PMID: 16669561]
- ARVD.com. The website of the Johns Hopkins ARVD Patient Registry based in Baltimore, Maryland.
- Hampton, JR. The ECG In Practice, 6e
- Mattu A, Brady W. ECG’s for the Emergency Physician 1
- Mattu A, Brady W. ECGs for the Emergency Physician 2
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric, 6e
- Wagner, GS. Marriott’s Practical Electrocardiography 12e
Further Reading
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
- Wiesbauer F. Little Black Book of ECG Secrets. Medmastery PDF
Acknowledgement
ECG 3 was originally posted on the website heartpearls.com by Dr Jayachandran Thejus MD. Thanks for sharing such a great ECG with us!
CLINICAL CASES
ECG EXIGENCY
Emergency Physician in Prehospital and Retrieval Medicine in Sydney, Australia. He has a passion for ECG interpretation and medical education | ECG Library |
