Ventricular Fibrillation (VF)
Ventricular fibrillation (VF) is the most important shockable cardiac arrest rhythm. It is invariably fatal unless advanced life support is rapidly instituted.
ECG findings in Ventricular Fibrillation (VF)
- Chaotic irregular deflections of varying amplitude
- No identifiable P waves, QRS complexes, or T waves
- Rate 150 to 500 per minute
- Amplitude decreases with duration (coarse VF –> fine VF)
Clinical significance of VF
Ventricular fibrillation (VF) is the most important shockable cardiac arrest rhythm.
- The ventricles suddenly attempt to contract at rates of up to 500 bpm
- This rapid and irregular electrical activity renders the ventricles unable to contract in a synchronised manner, resulting in immediate loss of cardiac output
- The heart is no longer an effective pump and is reduced to a quivering mess
- Unless advanced life support is rapidly instituted, this rhythm is invariably fatal
- Prolonged ventricular fibrillation results in decreasing waveform amplitude, from initial coarse VF to fine VF, ultimately degenerating into asystole due to progressive depletion of myocardial energy stores
Mechanism
In the presence of ischaemic heart disease VF may be preceded by:
- Premature ventricular contractions (PVCs)
- ST changes
- R on T phenomenon
- Sinus pause
- QT prolongation
- Ventricular tachycardia
- Supraventricular arrhythmias
- Sinus tachycardia
The underlying mechanism of VF is not fully understood. Several mechanisms have been hypothesised:
- Multiple wavelet mechanism: Multiple small wandering wavelets are formed, and the fibrillation is maintained by re-entry circuits formed by some of these wavelets
- Mother rotor mechanism: A stable re-entry circuit is formed, the ‘mother rotor’. The ‘mother rotor’ then gives rise to propagating unstable ‘daughter’ wavefronts, which results in the chaotic electrical activity seen on the ECG. Animal models suggest in any instance of VF there may be one or multiple ‘mother rotors’
Causes of Ventricular Fibrillation (VF)
Cardiac
- Myocardial ischemia / infarction
- Cardiomyopathy (dilated, hypertrophic, restrictive)
- Channelopathies e.g. Long QT (acquired / congenital) causing TdP –> VF and Brugada syndrome
- Aortic stenosis
- Aortic dissection
- Myocarditis
- Cardiac tamponade
- Blunt trauma (Commotio Cordis)
Respiratory
- Tension pneumothorax
- Pulmonary embolism
- Primary pulmonary hypertension
- Sleep apnoea
- Bronchospasm
- Aspiration
Toxic and Metabolic
- Drugs (e.g. verapamil in patients with AF+WPW)
- Drug-induced QT prolongation with torsades de pointes
Environmental
- Electrical shocks, drowning, hypothermia
- Sepsis
Neurological
- Seizure
- CVA
ECG Examples of VF
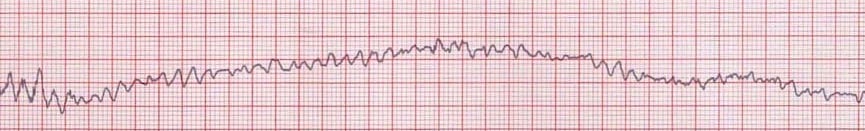
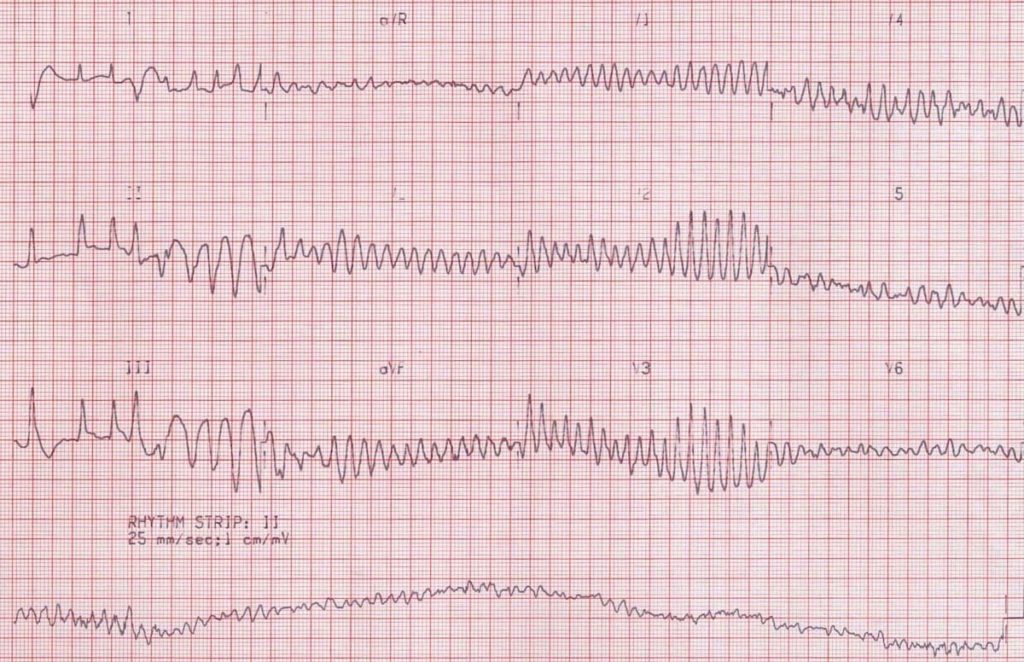
Example 1
- Typical rhythm strip of VF
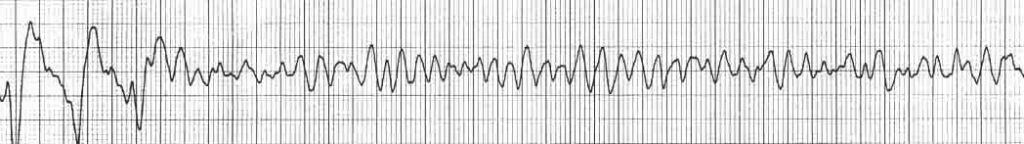
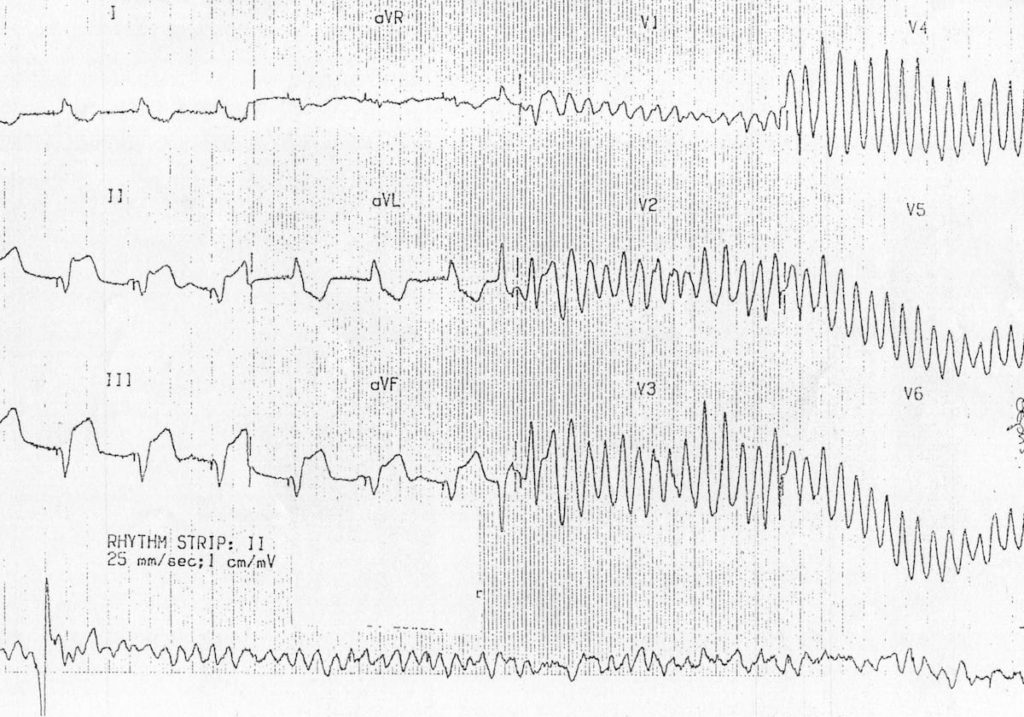
Example 2
- Appearance of fine VF
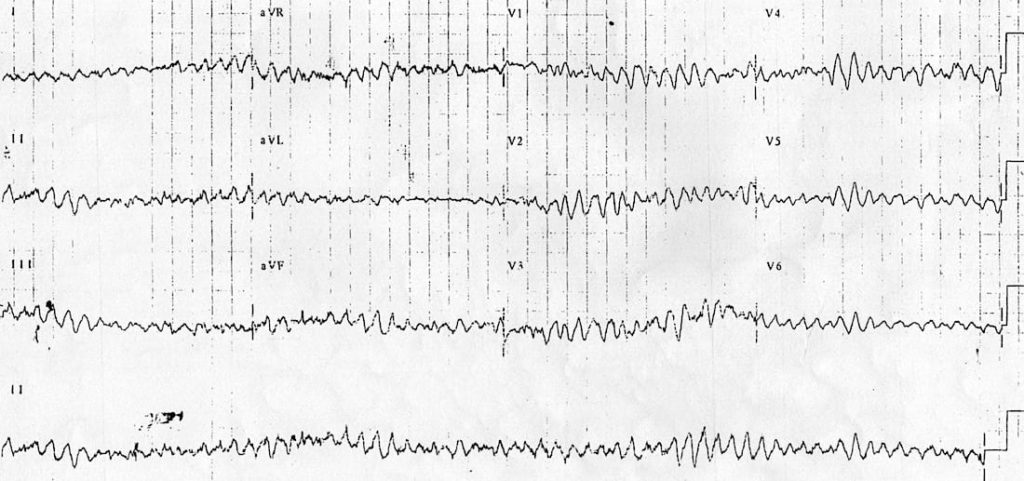
Example 3
- VF should never be diagnosed from the 12-lead ECG!
Example 4
- “R on T” phenomenon causing Torsades de Pointes, which subsequently degenerates to VF
- Notice that in this case the rhythm strip was recorded after the standard 12 leads — most ECG machines record them simultaneously
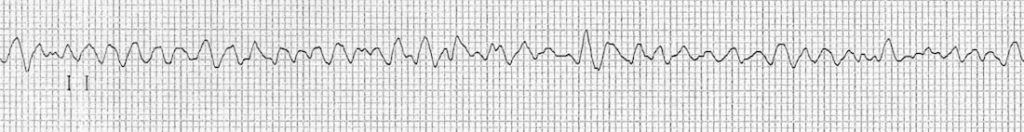
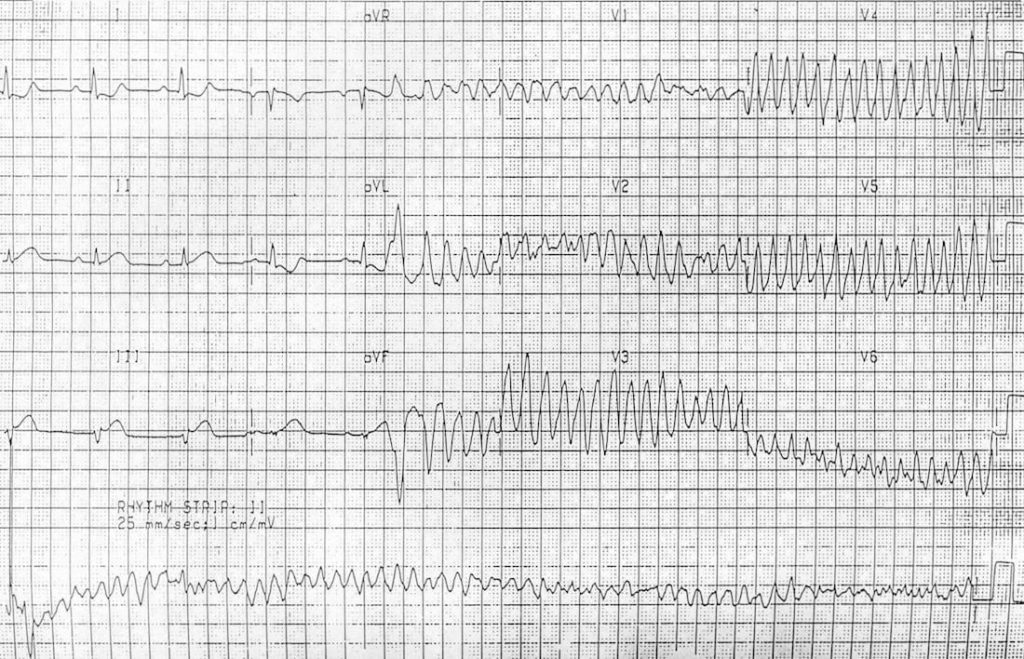
Example 5
- R on T leads to polymorphic VT, which then degenerates to VF
- The inferior ST elevation in the first part of the ECG may represent either inferior STEMI or simply the effects of ventricular pacing. Note the small pacing spikes in front of each QRS complex
- The magnitude of ST elevation suggests that this is an inferior STEMI in a paced patient (see Sgarbossa’s criteria)
- Again, the rhythm strip is recorded after the standard 12 leads.
and another example…
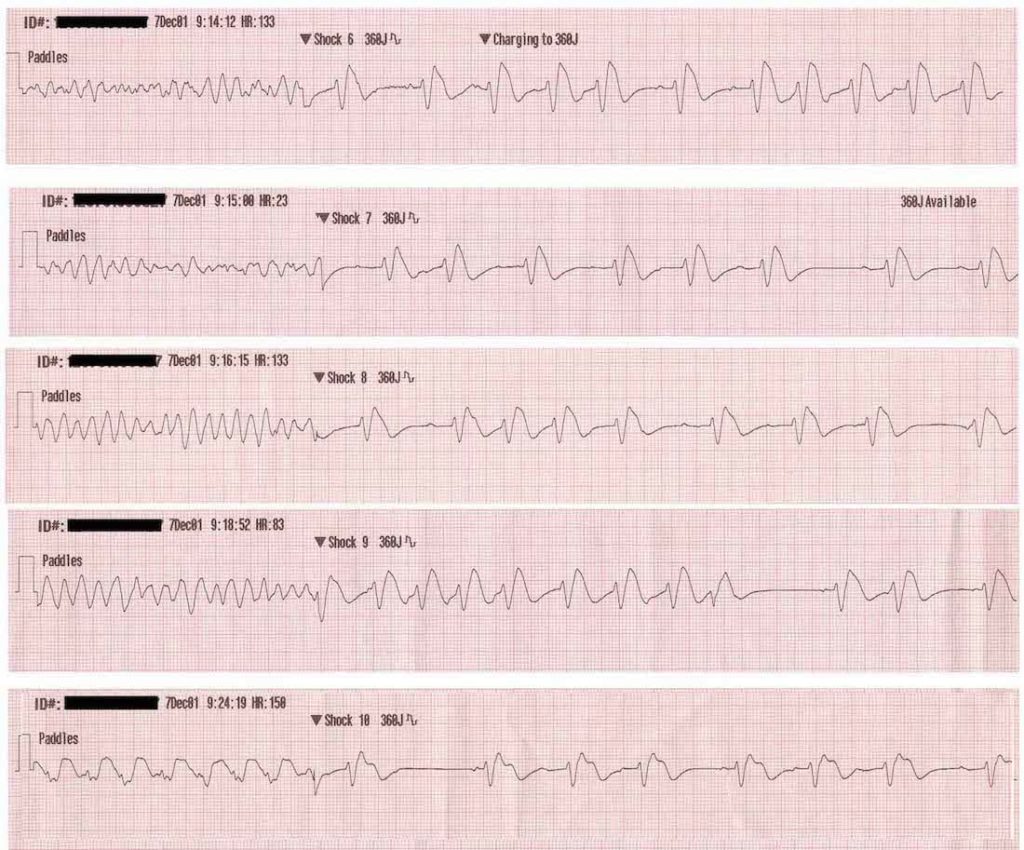
Example 6
- This patient is shocked out of VF five times in ten minutes!
- The subsequent rhythm in each case appears to be an accelerated idioventricular rhythm (broad QRS with AV dissociation), possibly with some fusion complexes in the second and third rhythm strips
Related Topics
References
- Da Costa D, Brady WJ, Edhouse J. Bradycardias and atrioventricular conduction block. BMJ. 2002 Mar 2;324(7336):535-8
- Ideker RE, Rogers JM. Human ventricular fibrillation: wandering wavelets, mother rotors, or both? Circulation. 2006 Aug 8;114(6):530-2.
- Nash MP, Mourad A, Clayton RH, Sutton PM, Bradley CP, Hayward M, Paterson DJ, Taggart P. Evidence for multiple mechanisms in human ventricular fibrillation. Circulation. 2006 Aug 8;114(6):536-42
- ten Tusscher KH, Mourad A, Nash MP, Clayton RH, Bradley CP, Paterson DJ, Hren R, Hayward M, Panfilov AV, Taggart P. Organization of ventricular fibrillation in the human heart: experiments and models. Exp Physiol. 2009 May;94(5):553-62.
Advanced Reading
Online
- Wiesbauer F, Kühn P. ECG Mastery: Yellow Belt online course. Understand ECG basics. Medmastery
- Wiesbauer F, Kühn P. ECG Mastery: Blue Belt online course: Become an ECG expert. Medmastery
- Kühn P, Houghton A. ECG Mastery: Black Belt Workshop. Advanced ECG interpretation. Medmastery
- Rawshani A. Clinical ECG Interpretation ECG Waves
- Smith SW. Dr Smith’s ECG blog.
Textbooks
- Zimmerman FH. ECG Core Curriculum. 2023
- Mattu A, Berberian J, Brady WJ. Emergency ECGs: Case-Based Review and Interpretations, 2022
- Straus DG, Schocken DD. Marriott’s Practical Electrocardiography 13e, 2021
- Brady WJ, Lipinski MJ et al. Electrocardiogram in Clinical Medicine. 1e, 2020
- Mattu A, Tabas JA, Brady WJ. Electrocardiography in Emergency, Acute, and Critical Care. 2e, 2019
- Hampton J, Adlam D. The ECG Made Practical 7e, 2019
- Kühn P, Lang C, Wiesbauer F. ECG Mastery: The Simplest Way to Learn the ECG. 2015
- Grauer K. ECG Pocket Brain (Expanded) 6e, 2014
- Surawicz B, Knilans T. Chou’s Electrocardiography in Clinical Practice: Adult and Pediatric 6e, 2008
- Chan TC. ECG in Emergency Medicine and Acute Care 1e, 2004
LITFL Further Reading
- ECG Library Basics – Waves, Intervals, Segments and Clinical Interpretation
- ECG A to Z by diagnosis – ECG interpretation in clinical context
- ECG Exigency and Cardiovascular Curveball – ECG Clinical Cases
- 100 ECG Quiz – Self-assessment tool for examination practice
- ECG Reference SITES and BOOKS – the best of the rest
[cite]
ECG LIBRARY
Emergency Physician in Prehospital and Retrieval Medicine in Sydney, Australia. He has a passion for ECG interpretation and medical education | ECG Library |
MBBS (UWA) CCPU (RCE, Biliary, DVT, E-FAST, AAA) Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Editor-in-chief of the LITFL ECG Library. Twitter: @rob_buttner


What do you mean by the statement on ECG Example 3. that “VF should never be diagnosed on a 12 lead ECG”. I think it is misleading. Please explain
Hi Kansiime,
I think Drs Buttner and Burns are referring to the fact that unless you already have a 12 lead ECG on the patient and accidentally capture someone developing VF (as seen in the R on T in ECGs 4 and 5 on the page) then you are wasting precious ALS time by applying a 12 lead ECG, and you should be able to diagnose VF on a standard rhythm strip/3 lead ECG. So I would take this statement as “tongue-in-cheek”.
I hope this answers your question / addresses your concerns!
James