Sulfa Drug Discombobulation
aka Immunological Inquisition 002
You’ve just diagnosed your patient with congestive heart failure and are about to give him a dose of frusemide, when you remember he has an allergy to sulfa drugs.
“Hmm, doesn’t frusemide contain a sulfa moiety?”, you ask yourself as you scratch your head, feeling slightly immunologically discombobulated.
[NB. the International non-propriety name for frusemide is furosemide]
Questions
Q1. What is frusemide’s mechanism of action?
Answer and interpretation
Frusemide is a loop diuretic.
Frusemide inhibits NKCC2, the luminal Na-K-2Cl symporter in the thick ascending limb of the loop of Henle. This results in decreased reabsorption of Na, K and Cl and concomitant diuresis. Excessive frusemide use is characterised by a hypokalemic hypochloremic metabolic alkalosis.
The effect of loop diuretics of the Na-K-2Cl symporter also abolishes the gradient required for the reabsorption of Mg and Ca. Thus hypomagnesemia and hypocalcemia can occur with frusemide use, though the latter is less common as Ca is actively reabsorbed in the distal convoluted tubule.
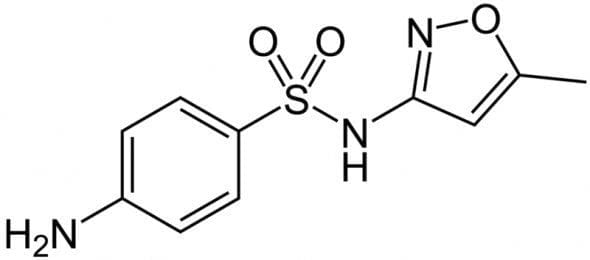
Q2. Does frusemide contain a sulfa moiety?
Q3. What other non-antibiotic drugs are ‘sulfa drugs’?
Answer and interpretation
There are lots of sulfa drugs around (this list is not exhaustive!) — some of them may surprise you!
Diuretics
- carbonic anhydrase inhibitors — acetazolamide
- loop diuretics — e.g. frusemide, budenoside
- thiazide diuretics — e.g. hydrochlorothiazide, indapamide, metalozone
Sulfonylureas
- chlopropramide
- glipizide
- tolbutamide
Rheumatological agents
- sulfasalazine
- probenicid
- celecoxib (NB. rofecoxib is not a sulfa drug)
Other agents
- sumatriptam
- topiramate
- ibutilide
- sotalol
- dapsone
Q4. What reactions may occur in patients with a ‘sulfa drug’ allergy?
Answer and interpretation
Adverse reactions to sulphonamide antibiotics are relatively common (~3%), but only about 3% of these are true hypersensitivity reactions.
The most common manifestation of hypersensitivity is a fever or a maculopapular rash that develops 7 to 14 days after initiating the offending agent. However, there are several life-threatening manifestations of hypersensitivity to sulfa drugs. These include:
- Stevens-Johnson syndrome
- toxic epidermal necrolysis
- agranulocytosis
- hemolytic anemia
- thrombocytopenia
- fulminant hepatic necrosis
Unfortunately, there is no reliable test for sulfa drug allergy.
Q5. Can you give frusemide to a patient with a ‘sulfa drug’ allergy?
Answer and interpretation
Yes, but…
Frusemide, like other non-antibiotic sulfa drugs lack the specific moieties present in antibiotic sulfa drugs (sulphonamides) that are thought to mediate hypersensitivity. These moieties are:
- the N1 heterocyclic ring — causes type I hypersensitivity reactions.
- the N4 amino nitrogen — results in reactive metabolites that cause either direct cytotoxicity or an immunologic response.
The best evidence available concerning sulfa drug cross-reactivity is probably Strom et al’s (2003) retrospective cohort study. These investigators studied 969 patients who had allergic reactions to sulfonamide antibiotics, and 19257 patients who had not, who subsequently received sulfonamide nonantibiotics. Using a very broad definition of ‘allergy’ patients allergic to sulfonamide antibiotics were more likely than nonallergic patients to react to sulfonamide nonantibiotics (9.9% vs 1.1%). However, there was an even higher rate among patients with documented penicillin allergy (14.2%)! Thus it is more likely that a reaction is related to a greater predisposition to allergic reactions in general among these patients rather than any specific sulfa hypersensitivity.
Expert opinion suggests that cross-reactivity between antibiotic sulfa drugs and non-antbiotic sulfa drugs is extremely unlikely.
Incidentally, there has only been one reported case of anaphylaxis to frusemide, and it could not be determined if the sulfa moiety was responsible.
Ponka (2006) summarises the approach to the problem of non-antibiotic sulfa drugs in patients with ‘sulfa drug allergy’ a bit like this:
- Is there a history of severe or life-threatening sulfa allergy?
YES —> do NOT give a non-antibiotic sulfa drug except in an emergency and there are no available alternatives.
NO —> ask the next question… - Is there a history of allergy to non-antibiotic sulfa drugs?
YES —> do NOT give a non-antibiotic sulfa drug except in an emergency and there are no available alternatives.
NO —> give a ‘test dose’ in a monitored setting after appropriate patient counseling, or use an available alternative.
Always seek the opinion of an allergist/ immunologist first.
Some additional comments:
Ponka’s approach is cautious. From what we know of the pharmacology mediating antibiotic sulfa drug hypersensitivity and the limited evidence available, there is no reason to suspect that there should be cross-reactivity with non-antibiotic sulfa drugs. However, absence of evidence is not the same as evidence of absence…
I am not aware of any established protocols describing how to give a ‘test dose’ in this situation. I suspect that the risk is sufficiently low (when there is no history of a severe sulfa drug reaction, and no history of a reaction to a non-antibiotic sulfa drug) that the usual treatment dose could be given followed by a period of close observation. A more cautious approach (as suggested by Daman Langguth, see comments below) would be to give 1/10th of the usual dose.
Finally, it is rare that a sulfa drug ever needs to be given as a true emergency.
Q6. What alternatives are there to frusemide?
Answer and interpretation
Ethacrynic acid
This drug is a non-sulfa containing loop diuretic. The dose is 50-200mg once or twice daily (50mg has a similar diuretic effect to 40mg frusemide). Like frusemide it is potentially ototoxic and hypokalemia is the main side effect — and it also causes diuresis over about 6 hours (hence the trade-name ‘lasix’ for frusemide: ‘lasts six hours’).
Rare side-effects of ethacrynic acid are:
- GI toxicity (nausea, vomiting, diarrhoea, GI haemorrhage)
- CNS effects: hallucinations, inappropriate behaviour, mania
- It is an ADEC category C drug with respect to pregnancy due to risk of neonatal thrombocytopenia and electrolyte disturbance.
Also, it should be noted that the potassium-sparing diuretics (triamterene, spironolactone, and amiloride) do not contain a sulfa-moiety and are also an option.
References
- Ponka D. Approach to managing patients with sulfa allergy: use of antibiotic and nonantibiotic sulfonamides. Can Fam Physician. 2006 Nov;52(11):1434-8. PMID: 17279201; PMCID: PMC1783707.
- Strom BL, Schinnar R, Apter AJ, Margolis DJ, Lautenbach E, Hennessy S, et al. Absence of cross-reactivity between sulfonamide antibiotics and sulfonamide nonantibiotics. N Engl J Med. 2003;349:1628–1635. PMID: 14573734
- Wulf NR, Matuszewski KA. Sulfonamide cross-reactivity: is there evidence to support broad cross-allergenicity? Am J Health Syst Pharm. 2013 Sep 1;70(17):1483-94. doi: 10.2146/ajhp120291. PubMed PMID: 23943179.

CLINICAL CASES
Immunological Inquisition
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC