Temporomandibular joint and headache
Recognizing temporomandibular joint issues
There are several oral structures that can cause referred pain. The temporomandibular joint (TMJ) is often affected by intraarticular dysfunction which can lead to an abnormality in the way the teeth meet (referred to as malocclusion). Chewing will exacerbate this dysfunction.
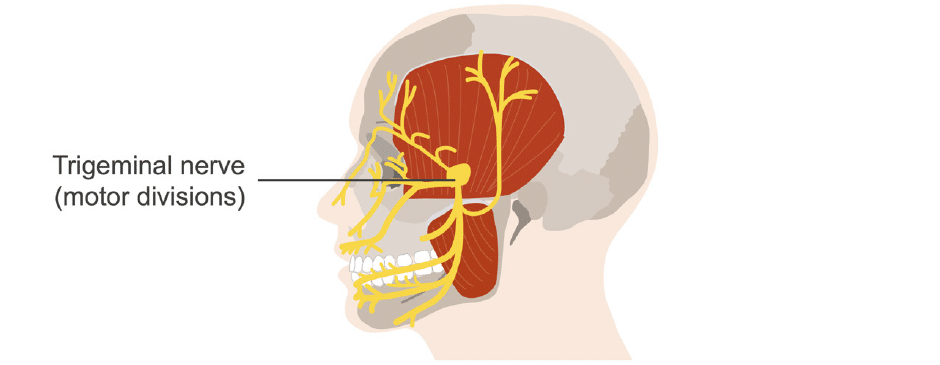
The masseter and temporalis muscles are responsible for opening and closing the jaw during chewing. These muscles are innervated by the motor divisions of the trigeminal nerve.
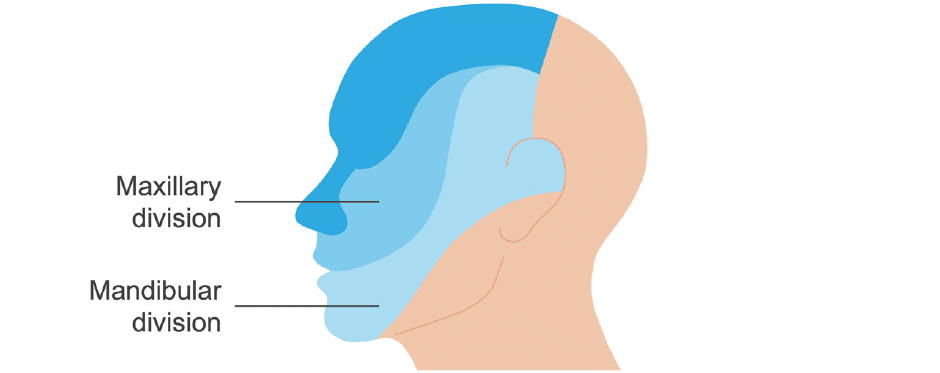
Two divisions of the trigeminal nerve mediate dental pain: the mandibular and maxillary divisions. These nerves carry pain impulses from the teeth and other regional structures (e.g., the salivary glands), and non-dental processes subserved by these nerves can refer pain to the teeth.
TMJ disorders
TMJ disorders can have components of joint dysfunction and muscular dysfunction. Joint dysfunction encompasses disc and ligamental dysfunction or arthritic changes associated with pain in the joint itself.
Muscular dysfunction refers to pain in the muscles of mastication that is worsened with chewing. Aggravation of either form occurs when the jaw is put into functional motion. TMJ movement may be accompanied with a click, locking, and / or asymmetrical movement (seen as translation with jaw opening).
What causes TMJ pain?
Parafunctional activities have been implicated but not proven to be a definitive aetiology for TMJ pain. Unlike functional activities such as chewing and eating, parafunctional activities are defined as abnormal, typically hyperactive functions of the masticatory structures, including the tongue, teeth, and oral muscles. Examples include bruxism (teeth grinding), jaw clenching, and thumb sucking.
It is often noted that parafunctional behaviors are common, yet headache does not occur in all patients who exhibit them. So, other mechanisms may be responsible for activating headaches in this population of patients. It is not known if the parafunction is overworking the muscles or if there could be some other central nervous system mechanism responsible, perhaps central sensitisation.
Of interest, most patients with headaches and these parafunctional behaviors are often younger, pointing to a more complicated system. The controversy suggests that more research is needed.
Identifying the cause of TMJ pain
To identify parafunctional activities or oromandibular dysfunction as a cause for headache, observe the teeth for signs of wear, such as rounding of ridges and flattening of surfaces. Other signs include retraction of the gums, tooth impressions on the tongue, tenderness of the temporalis and masseter muscles with trigger points, and tenderness at or around the mastoid process.
Recall that bruxism and trigger points may also cause migraines.
Treating TMJ pain
In terms of treatment, oral appliance therapy can protect the teeth and is sometimes effective headache therapy. Presumably, this works by having some effect directly on the masticatory muscles, particularly the temporalis muscle, or by some feedback mechanism.
Medications such as tricyclic antidepressants and anti-inflammatory drugs, and behavioral therapy, can be also be helpful.
This is an edited excerpt from the Medmastery course Headache Masterclass by Robert Coni, DO, EdS, FAAN. Acknowledgement and attribution to Medmastery for providing course transcripts.
- Coni R. Headache Masterclass. Medmastery
- Coni R. Clinical Neurology Essentials. Medmastery
- Simmonds GR. Neurology Masterclass: Managing Common Diseases. Medmastery
- Simmonds GR. Neurology Masterclass: Managing Emergencies. Medmastery
References
- The International Classification of Headache Disorders 3rd edition
- Cashman EC, Smyth D. Primary headache syndromes and sinus headache: An approach to diagnosis and management. Auris Nasus Larynx. 2012 Jun;39(3):257-60.
- Chou DE. Secondary Headache Syndromes. Continuum (Minneap Minn). 2018 Aug;24(4, Headache):1179-1191
- Do TP, Heldarskard GF, Kolding LT, Hvedstrup J, Schytz HW. Myofascial trigger points in migraine and tension-type headache. J Headache Pain. 2018 Sep 10;19(1):84
- Graff-Radford SB. Facial pain, cervical pain, and headache. Continuum (Minneap Minn). 2012 Aug;18(4):869-82.
- Tepper SJ. Cranial Neuralgias. Continuum (Minneap Minn). 2018 Aug;24(4, Headache):1157-1178.
- Tsakadze, N, Antonovich N, Rossi F. Medication-overuse headache. Practical Neurology. 2018; 17: 50–52.
- Armand CE, Masters-Israilov A, Lipton RB. Migraine mimics. Practical Neurology. 2019; 18: 32–39
Neurology Library: Secondary headaches
- Coni R. Sinus headaches. LITFL
- Coni R. Muskuloskeletal pain and headache. LITFL
- Coni R. Temporomandibular joint and headache. LITFL
Neurology Library
Robert Coni, DO, EdS, FAAN. Vascular neurologist and neurohospitalist and Neurology Subspecialty Coordinator at the Grand Strand Medical Center in South Carolina. Former neuroscience curriculum coordinator at St. Luke’s / Temple Medical School and fellow of the American Academy of Neurology. In my spare time, I like to play guitar and go fly fishing. | Medmastery | Linkedin |
BMBS (The University of Nottingham) BMedSci (The University of Nottingham). Emergency Medicine RMO at Sir Charles Gairdner Hospital Perth, WA. Interested in Medical Education and Emergency Medicine. Swimmer and frequent concert attendee.


