Migraine headache
Recognising migraine headaches
Migraine is a complex neurophysiological disease characterized by episodic, and sometimes chronic, and progressive forms of headache. There are associated neurologic and non-neurologic symptoms that accompany the head pain.
Note that the International Headache Society classification for migraine include: migraine without aura, migraine with aura, chronic migraine and associated migraine complications. Additionally, there are separate categories for gastrointestinal symptoms and vertigo which can be associated with migraine.
Basic diagnostic criteria for migraine
All International Classification of Headache Disorders criteria always include a statement that in order to apply a certain diagnosis, the syndrome must not be better accounted for by any other diagnosis.
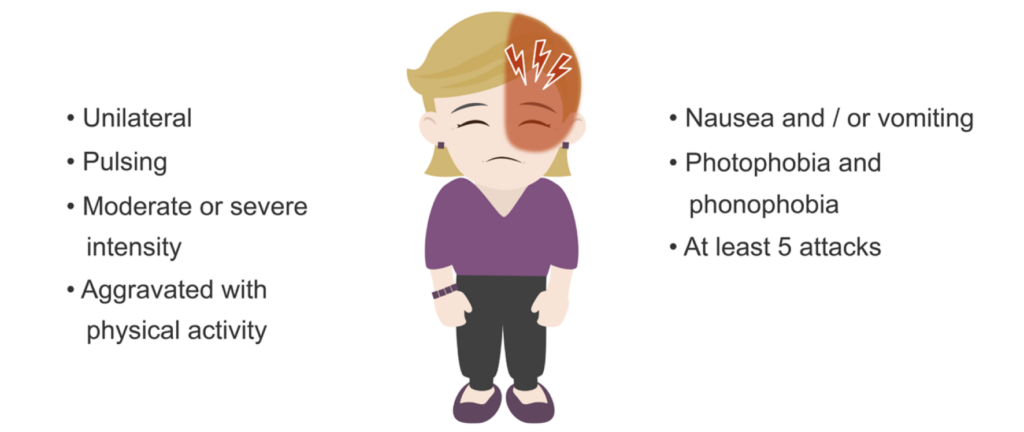
There are four basic diagnostic criteria for all migraine types:
- The headache will last 4– 72 hours if left untreated or unsuccessfully treated.
- The headache has at least two of the following four characteristics:
- Unilateral location
- Pulsating quality
- Moderate or severe pain intensity
- Aggravated by routine physical activity such as walking or climbing stairs or the migraine sufferer will avoid these activities.
- During a migraine headache, at least one of the following is present:
- Nausea and / or vomiting
- Photophobia and phonophobia
- Finally, there should be a history of at least five attacks having occurred which fulfill the above criteria.
Diagnostic criteria for migraine with aura
For migraine that occurs with an aura, there are several other criteria that must be met for a diagnosis. Remember that an aura refers to a group of symptoms—visual, sensory, or other central nervous system symptoms—which are fully-reversible, and develop gradually:
- Visual changes such as spots, clouded fields, flashes of light or scintillations
- Sensory symptoms such as numbness or pins and needles
- Speech and / or language dysfunction
- Motor power loss
- Brainstem dysfunction such as diplopia, dizziness, or facial sensory changes

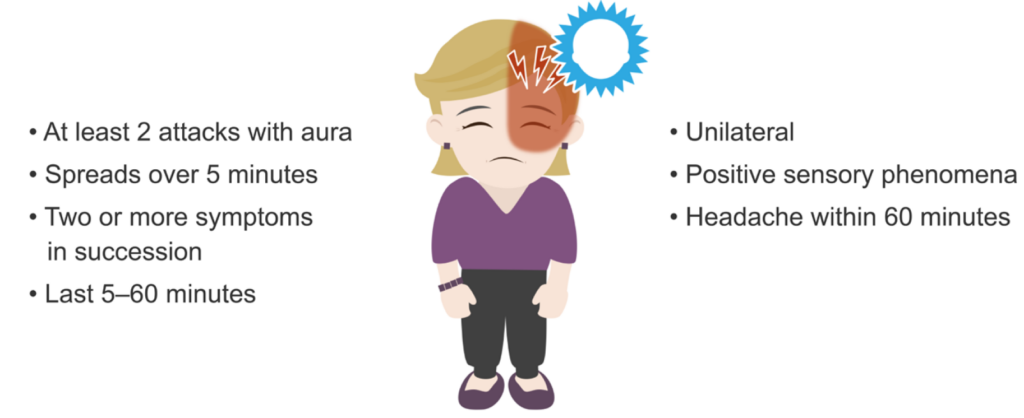
In addition to all of the basic migraine criteria, there are several others that must be fulfilled to diagnose migraine with aura:
- There must be at least two attacks that have any of the symptoms of aura above.
- Aura symptoms must have at least three of the following six characteristics:
- At least one aura symptom spreads gradually over five minutes
- Two or more aura symptoms occur in succession
- Each individual aura symptom lasts 5–60 minutes
- At least one aura symptom is unilateral
- At least one aura symptom is positive, meaning a symptom of an added sensory perceptive phenomena such as scintillating lights or pins and needles
- The aura is accompanied, or followed within 60 minutes, by a headache
Additional criteria to diagnose migraine with aura
Non-diagnostic criteria of migraine
Migraine headaches have a female to male gender ratio of approximately 3:1. There are many comorbid conditions with migraine, including depression, anxiety, sleep disorders, and obsessive-compulsive disorder.
There may be a genetic predisposition to migraine. Those predisposed typically can identify triggering mechanisms such as certain foods, weather changes, fasting, sleep disturbances, stress, and hormonal fluctuations.
There are also migraines which provoke neurologic dysfunction known as complicated migraines. One example is a form of migraine called a hemiplegic migraine which will produce neurologic dysfunction, appearing as stroke-like symptoms, on one side of the body. These events run in families, and testing can be done to determine if genetic human leukocyte antigen (HLA) types associated with the syndrome are present.
The four stages of migraine
There are four phases to a migraine:
- Prodrome phase
- Aura phase
- Pain (or headache) phase
- Resolution phase
Phase 1: Prodrome
A prodrome is an indication of an impending migraine attack. Generally, patients will experience a prodrome that they recognise as such. The prodromal phase usually occurs one to three days before the attack.
Many patients describe a change in mood, while others describe a change in behavior. Many patients describe the feeling that they are going to get a headache. Some describe depression, others cognitive slowing, and food cravings.
Phase 2: Aura
Some patients will experience a migraine aura. Auras are generally a symptom complex associated with focal neurologic phenomena and may be either positive or negative symptoms. Positive symptoms refer to some added perception; for instance, zigzag lines appearing in the vision or experiencing a sensation of pins and needles. Negative symptoms include loss of some neurologic function; for instance, weakness or vision loss.
Auras generally develop over 5 to 15 minutes, and usually resolve within an hour.
The most typical auras are elementary visual disturbances:
- Scotoma (a localized visual field deficit surrounded by areas of normal vision)
- Seeing clouds
- Seeing spots
- Flashes
- Geometric shapes (e.g., zigzag lines, or fortification spectra)
Visual auras obscure part or all of the visual field, and they may cross the visual field and enlarge.
Alterations of visual perception may also occur:
- Metamorphopsia (a distortion of vision)
- Micropsia (a reduction of the apparent image size)
- Macropsia (an enlargement of the apparent image size)
- Mosaics (a kaleidoscope effect)
More complicated auras include the following:
- Paresthesias
- Perception difficulties • Apraxia (the inability to perform a learned task)
- Speech and language dysfunction
- Déjà vu or jamais vu
- Some degree of motor dysfunction (e.g., sensory ataxia)
At the resolution of the aura, the pain or headache phase will begin, generally within an hour.
Phase 3: Pain / headache
A migraine headache is typically unilateral, throbbing in character, and moderate to severe in intensity. The pain is aggravated by physical activity. Sometimes the pain is bilateral, either starting that way and progressing to become unilateral, or vice versa. The pain phase will generally last from a few hours to three days.
Associated symptoms include:
- Anorexia
- Nausea
- Vomiting
- Sensitivity to light and sound
- Smells may be poorly tolerated
The headache phase is generally the result of the activation of meningeal and blood vessel pain receptors by neurotransmitters and peptides released centrally and acting through the trigeminal nerve connections to these pain receptors. Sometimes these centrally acting neurotransmitters and peptides further enhance pain in a process called secondary sensitization. These released chemical mediators ultimately result in inflammation, vasodilation, protein extravasation and platelet activation.
This neurogenic inflammation can then sensitise nerve fibres, a process called peripheral sensitisation. These activated fibres will be triggered by normally mild stimuli, such as blood vessel pulsations, creating hyperalgesia, or allodynia. In other words, the process of peripheral sensitisation results in pain.
Note: Sometime the headache phase of the migraine does not occur. This is termed acephalgic migraine or migraine equivalent.
Phase 4: Resolution
During the resolution phase, the pain decreases and gradually resolves. The patient may feel tired, irritable, and cognitively clouded. There may also be residual scalp allodynia, which can continue even after the headache resolves.
This is an edited excerpt from the Medmastery course Headache Masterclass by Robert Coni, DO, EdS, FAAN. Acknowledgement and attribution to Medmastery for providing course transcripts.
- Coni R. Headache Masterclass. Medmastery
- Coni R. Clinical Neurology Essentials. Medmastery
- Simmonds GR. Neurology Masterclass: Managing Common Diseases. Medmastery
- Simmonds GR. Neurology Masterclass: Managing Emergencies. Medmastery
References
- The International Classification of Headache Disorders 3rd edition
- Ward TN. Migraine diagnosis and pathophysiology. Continuum (Minneap Minn). 2012 Aug;18(4):753-63.
Neurology Library: The primary headache disorders
- Coni R. Deconstructing headache classification. LITFL
- Coni R. Headache aetiology. LITFL
- Coni R. Migraine headache. LITFL
- Coni R. Tension headache. LITFL
- Coni R. Cluster headache. LITFL
- Coni R. Trigeminal autonomic cephalalgias. LITFL
- Coni R. Other primary headaches. LITFL
- Coni R. Chronic daily headaches. LITFL
Neurology Library
Robert Coni, DO, EdS, FAAN. Vascular neurologist and neurohospitalist and Neurology Subspecialty Coordinator at the Grand Strand Medical Center in South Carolina. Former neuroscience curriculum coordinator at St. Luke’s / Temple Medical School and fellow of the American Academy of Neurology. In my spare time, I like to play guitar and go fly fishing. | Medmastery | Linkedin |
BMBS (The University of Nottingham) BMedSci (The University of Nottingham). Emergency Medicine RMO at Sir Charles Gairdner Hospital Perth, WA. Interested in Medical Education and Emergency Medicine. Swimmer and frequent concert attendee.


