Tetraology of Fallot and BT shunts
aka Cardiovascular Curveball 009
Despite the therapeutic measures described in Pediatric Perplexity 003 the 26 day-old boy with Tetralogy of Fallot and severe hypercyanotic spells is in dire straits.
He has been intubated and requires mechanical ventilation in conjunction with a phenylephrine infusion in order to achieve arterial oxygenation compatible with life. The decision is made to perform life-saving cardiac surgery.
Questions
Q1. What are the surgical options for Tetralogy of Fallot?
Curveball Answer
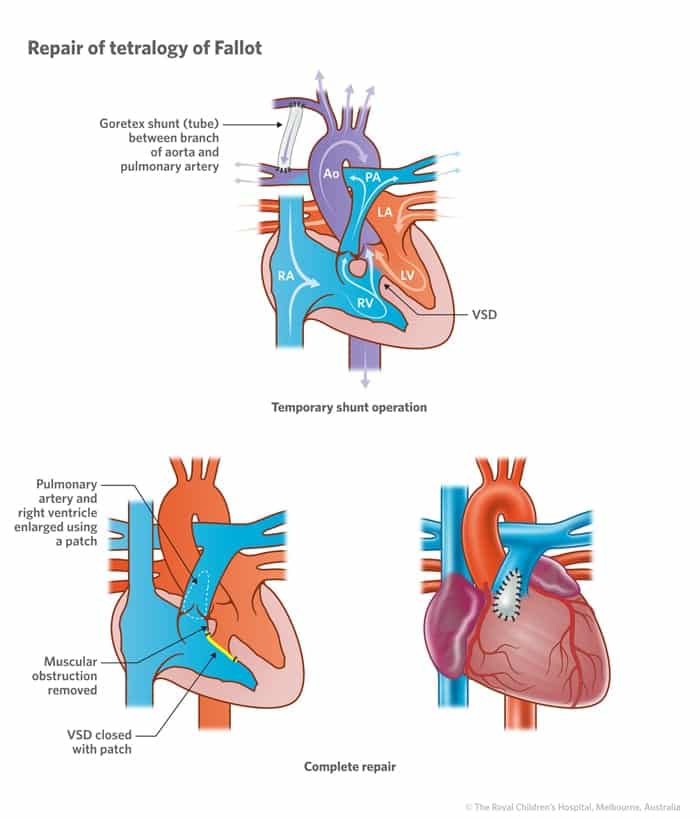
Options include formation of a modified Blalock-Tausig (BT) shunt or definitive repair.
- The occurrence of ‘tet spells’ is generally an indication for cardiac surgery, at least in the long term. Surgery may be palliative or corrective.
- Elective repair in relatively asymptomatic children is usually performed at about 6 months of age. Definitive repair has about 95% survival at 25 years, with the majority of patients living unrestricted adult lives.
The decision was made to perform a modified BT shunt in this child as the first stage pending definitive repair when the child is older.

Q2. What is a modified Blalock-Tausig shunt?
Curveball Answer
The modified BT shunt is a surgically-created (goretex) conduit between a subclavian artery and the pulmonary artery.
- It improves blood flow to the pulmonary circulation by providing a route for returning systemic blood that bypasses the right ventricular outflow obstruction.
- Following a modified BT shunt, arterial oxygen saturations of about 70 to 85% are optimal as they indicate relative balance between pulmonary and systemic blood flows.
- The original BT shunt operation was first performed in 1941 by Helen Tausig and Alfred Blalock. Marc De Leval later modified the procedure so that transection of the subclavian artery is not required.
- As if being recognized as the founder of pediatric cardiology wasn’t enough, Helen Tausig went onto play a major role in limiting the thalidomide disaster in the United States by bringing European reports of phocomelia to the attention of the FDA.
Q3. Describe the post-op ICU management of excessive hypoxia (e.g. SO2 60%)
Curveball Answer
Check blood pressure and ventilatory parameters, correct as needed
Rule out pulmonary disease (examination, ultrasound and CXR)
Suspect BT shunt malfunction:
- Auscultate for a shunt murmur
- Arrange urgent echocardiography to assess shunt flow
- Inform the cardiac surgeon
- Consider a heparin infusion (e.g. 10-20 U/kg/h) if high risk of shunt occlusion
- Consider increasing vasopressors to increase SVR as a temporizing measure
Q4. Describe the post-op ICU management of excessive oxygenation (e.g. SO2 95%)
Curveball Answer
Check and correct ventilatory parameters (e.g. high inspired O2)
Suspect ‘over-shunting’ (excessive pulmonary blood flow relative to systemic blood flow) if:
- SaO2>85% at low FiO2
- pulmonary plethora or pulmonary edema (can be unilateral)
- cardiac failure
- low systemic diastolic pressure (due to excessive ‘run off’ into the pulmonary circulation)
- persistent metabolic acidosis in a ‘pink’ patient (due to decreased systemic blood flow)
References
- Duncan A, Croston E. Guidelines for Intensive Care Management of Infants and Children after Congenital Heart Surgery. Pediatric Intensive Care Unit, Princess Margaret Hospital, 2008.
- Libby P, et al Braunwald’s Heart Disease A Textbook of Cardiovascular Medicine
CLINICAL CASES
Cardiovascular Curveball
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
