Tibial nerve lesions
Tibial nerve lesions cause plantarflexion weakness, sensory loss in the sole, and can result from trauma, compartment syndrome, or systemic neuropathy
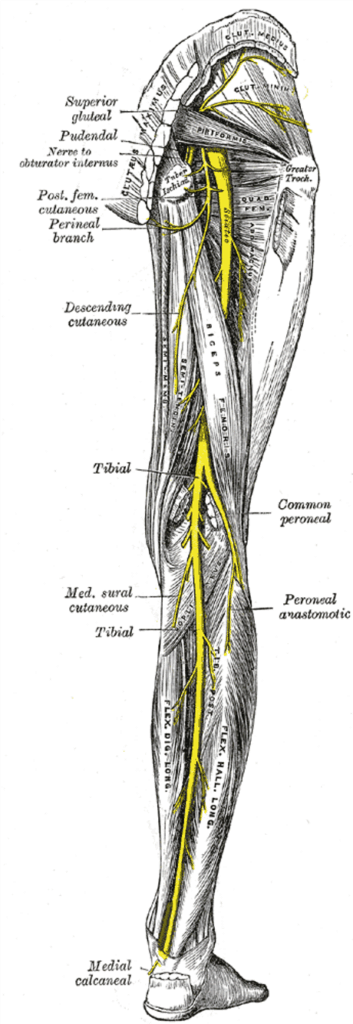
The tibial nerve provides motor innervation to the muscles of the posterior compartment of the leg (superficial and deep). It provides sensory innervation to the posterior aspect of the leg (via the sural nerve) and the sole of the foot.
Injury typically results in:
- Loss of plantar flexion of the foot and toes
- Weakened inversion of the foot
- Sensory loss over the posterior leg and sole of the foot
The tibial nerve is generally well protected by surrounding muscle but is most vulnerable in the popliteal fossa.
Anatomy
Course of the tibial nerve
- Arises from the sciatic nerve in the lower third of the thigh
- Derived from anterior divisions of L4–S3
- Travels through the popliteal fossa:
- Initially lateral to the popliteal artery
- Passes posterior to it at the knee
- Then medial to it at the level of the popliteus
- Vein lies between nerve and artery throughout
- Continues into the posterior leg deep to soleus
- Descends lateral to the posterior tibial artery
- At the ankle, passes posterior to the medial malleolus under the flexor retinaculum
Structures deep to the flexor retinaculum (anterior to posterior):
Mnemonic: Tom, Dick And Very Naughty Harry
- Tibialis posterior
- Flexor digitorum longus
- Posterior tibial artery
- Venae comitantes
- Tibial nerve
- Flexor hallucis longus
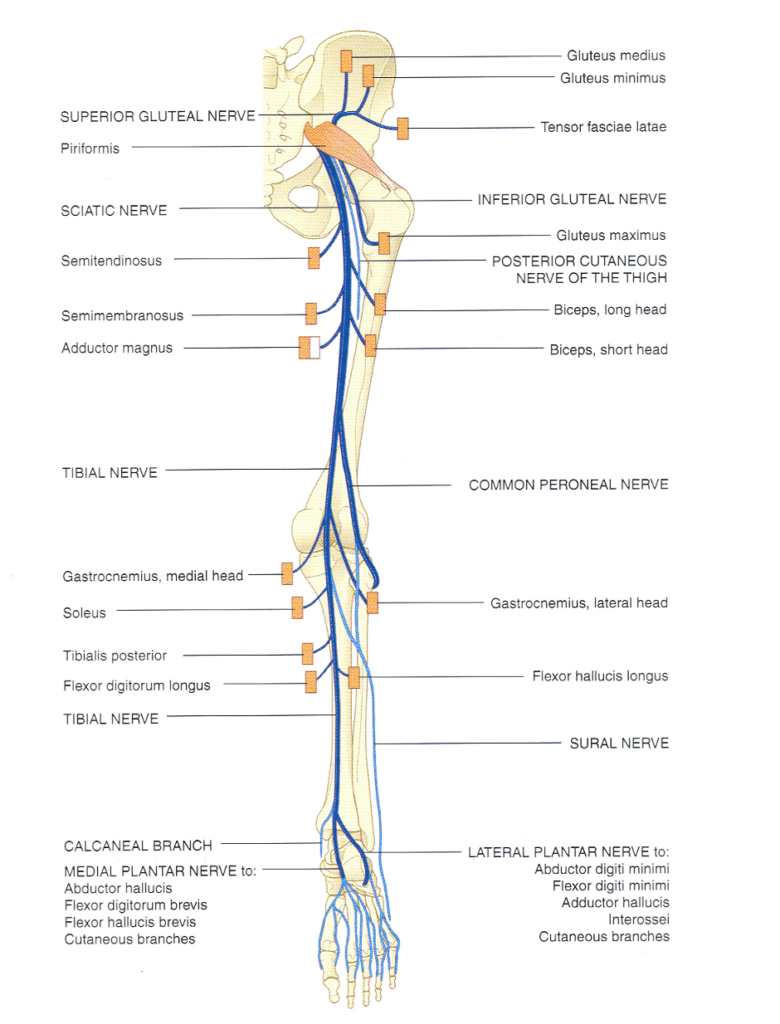
Tibial nerve innervations
In the popliteal fossa
Motor:
- Soleus
- Gastrocnemius
- Popliteus
- Plantaris
Sensory:
- Knee joint
- Medial sural cutaneous nerve → joins peroneal communicating nerve → sural nerve → supplies lateral foot to the 5th toe
Below the popliteal fossa
Motor:
- Flexor digitorum longus
- Flexor hallucis longus
- Tibialis posterior
Sensory:
- Ankle joint
- Medial calcaneal nerve → medial heel and plantar surface
Terminal branches at ankle
Medial plantar nerve
Motor:
- Abductor hallucis
- Flexor digitorum brevis
- Flexor hallucis brevis
- 1st lumbrical
Sensory:
- Medial sole and medial 3½ toes (including nail beds)
Lateral plantar nerve
- Runs with lateral plantar artery
- Divides at 5th metatarsal into superficial and deep branches
Main trunk motor:
- Quadratus plantae
- Abductor digiti minimi
Main trunk sensory:
- Lateral sole
Superficial branch:
- Motor: flexor digiti minimi brevis, 4th interosseous
- Sensory: lateral 1½ toes (including nail beds)
Deep branch:
- Adductor hallucis
- 2nd–4th lumbricals
- 1st–3rd interossei
Pathology
Causes of tibial nerve lesions
- Trauma
- Direct trauma to popliteal fossa or medial malleolus
- Knee dislocations
- Neuropraxias
- Posterior leg compartment syndrome
- Mass lesions
- Tumours
- Abscesses
- Neuropathies
- Mononeuropathies from systemic disease (rarely affects tibial nerve)
Clinical assessment
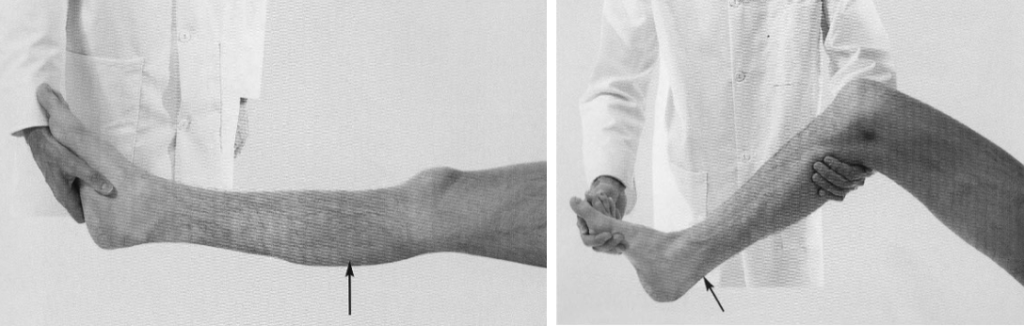
Right: testing Soleus (Tibial nerve, S1,2): the patient lies supine with the hip and knee flexed, while plantar flexing the foot against resistance. The muscle belly can be felt, and occasionally can also be seen.
Middle: testing flexor digitorum longus and flexor hallucis longus, (Tibial nerve L5, S1, S2): the patient is asked to flex the toes against resistance.
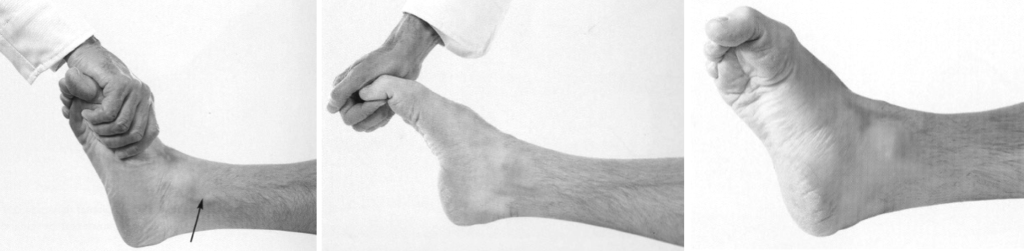
Right: Testing the medial and lateral plantar nerves: (S1,2) the patient is asked to cup the sole of the foot. Small muscles can be felt and sometimes seen

Middle: The approximate regions within which sensory changes may be found with lesions of the Tibial nerve.
Right: The sensory innervation of the sole of the foot
Investigations
Blood tests
- FBC
- U&Es / glucose
- CRP
- ESR
- Others (e.g. lead levels)
Imaging
- CT / MRI: to delineate compressive lesions or visualise the nerve
Nerve conduction studies
- Confirm diagnosis
- Exclude generalised disease
- Determine prognosis
Management
- Treat underlying cause
- Neuropraxia
- Fasciotomy for compartment syndrome
- Occupational therapy
- Splints and aids
- Physiotherapy
- Recovery and prevention of complications
Disposition
Depends on:
- Cause of lesion
- Symptom severity
- Acute vs chronic presentation
Appendix 1
Appendix 2
References
Publications
- Brazis PW, Masdeu JC, Biller J. Localization in Clinical Neurology. 8e 2021
- Fuller G. Neurological Examination Made Easy. 6e 2019
- O’Brien M. Aids to the Examination of the Peripheral Nervous System. 6e 2023
FOAMed
- Coni R. Neuro 101: Peripheral Nervous System. LITFL
- Nickson C. Myotomes and Differentiating Nerve Lesions. LITFL
Fellowship Notes
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner
Educator, magister, munus exemplar, dicata in agro subitis medicina et discrimine cura | FFS |


