Trauma! Are you prepared?
aka Trauma Tribulation 013
The bat phone rings…
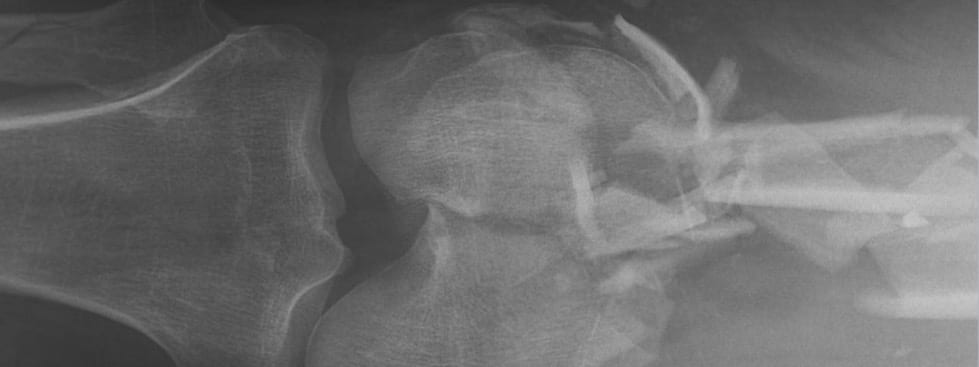
An ambulance is en route with a 35 year old male who was the restrained driver of a car that rolled into a ditch after swerving to avoid a dog. The front seat passenger died at the scene. The patient’s vitals are T36.1C, HR 100/min, RR 22/min, BP 105/70 mmHg, SpO2 98%OA and he is GCS 13 (E4 V3 M6). The paramedics state he has contusions to his forehead, a ‘seat belt’ sign, and a tender swelling of his right thigh.
The ETA is 10 minutes from now… Are you prepared?
Questions
Q1. What exactly is major trauma?
Answer and interpretation
It is possible to go through a few years of emergency medicine training without ever actually knowing the strict definition of major trauma…
In essence, major trauma — also known as ‘multiple trauma’ — refers to major injury affecting more than one body system. It can also be defined as an Injury Severity score > 15.
Q2. Should a trauma call go out?
Answer and interpretation
Yes — the mechanism is high risk (roll over with a death at the scene), he has markers of severe injury (seat belt sign, possible long bone fracture) and physiological derangement (especially decreased GCS).
Specific criteria for activation of a trauma call, or transfer to a trauma center, varies between hospitals and systems. Criteria are usually a combination of mechanism, specific injuries, physiological derangement, patient factors and physician discretion.
- Mechanism
— e.g. falls > 6m, high risk MVCs, MBCs, vehicle versus cyclist or pedestrian - Specific injuries
— e.g. flail chest, paralysis, proximal penetrating injuries or amputations, multiple long bone fractures, pelvic fractures, and crushed or mangled extremity. - Physiological derangement
— e.g. GCS <14, SBP <90 mmHg, RR >30 or <10/min - Patient factors
— e.g. extremes of age, pregnancy, bleeding diathesis.
Q3. What are the key steps in assessment and management of a major trauma patient?
Answer and interpretation
The key steps, according to ATLS principles (with a few additions and clarifications) are:
- Preparation, triage and activation of the trauma resuscitation team.
- Transfer the patient from the ambulance stretcher to the ED resuscitation bed using spinal injury precautions if indicated.
- Obtain a handover from prehospital care providers including history, including the mechanism of injury, field treatment, and response to treatment.
- Obtain vital signs while the patient is being undressed.
- Primary survey (ABCDE) and resuscitation as needed, while obtaining large bore IV access.
- Take blood tests for group and hold/ cross-match, and baseline laboratory testing (e.g. blood gas, Hb, coagulation studies)
- Adjuncts to primary survey and resuscitation
(IDC, NGT, ECG, monitoring, trauma X-ray series and bedside ultrasound) - Consider need for patient transfer
(initiate as soon as adequate information is available) - Secondary survey
- Adjuncts to the secondary survey
(further imaging and investigations) - Continued post-resuscitation monitoring and reevaluation
- Definitive care and disposition
Q4. What are the key things to prepare?
Answer and interpretation
ATLS (8th edition) describes 2 phases of preparation for major trauma: prehospital and hospital phases. Here, we are interested in the latter.
This simple set of headings is worth remembering when preparing for the ‘hospital phase’ management of any critically ill patient:
- People
- Place
- Equipment and drugs
People
- Consider trauma team activation
- Ensure continued safe running of the rest of the emergency department
- Patient and family may need social support.
- Security (especially if gunshot wound… someone might come to finish off the job)
- Notify other hospital areas as required (e.g. radiology, operating theatres, ICU, laboratory)
Place
- Ideally a designated trauma bay with facilitates for resuscitation
Equipment and drugs
- Anticipate what you might need, thinking through systems in an ABCDE approach
- For example: universal precautions, advanced airway equipment, analgesia and rapid sequence intubation drugs, chest tubes, rapid transfusers, activate massive transfusion protocol, pelvic binders, femoral splints, warming equipment, emergency thoracotomy tray.
Q5. Who makes up the Trauma Team and what are their roles?
Answer and interpretation
Team structures vary between systems and hospitals. In small centres the team may consist of only a doctor and a nurse. In trauma centres there are defined roles, and the team members assemble when activated by a trauma call.
More important than the composition of the trauma team is that the team members are trained in the emergency care of trauma patients and work effectively as a team with:
- clear roles and organization
- effective communication
- support from other hospital areas, transfer services and trauma centres
Team roles include:
- Team Leader — usually a senior emergency medicine doctor who coordinates assessment and management.
- Airway doctor — doctor with advanced airway skills (ED, anaesthetics or ICU)
- Procedures doctor — emergency doctor
- Assessment doctor — emergency doctor or surgical doctor
- Airway nurse — nurse trained to assist with advanced airway management
- Drugs/ procedures nurse(s) — nurse(s)s assist with
- Scribe — nurse who keeps a real time written record of events and interventions
- Runners — healthcare assistants who relay messages, source equipment and assist in transfers
In addition to the trauma/ general surgical doctor, other surgical specialties may be alerted to the trauma call as the scenario demands. These specialties may include orthopedics, neurosurgery, cardiothoracics, plastics, ENT and ophthalmology. Early notification of operating theatre staff and ICU is also crucial for critically ill trauma patients.
Notification of radiography and radiology staff is also a key part of trauma team activation. This ensures rapid access to diagnostic +/- interventional radiology and allows rapid decision making.
In some centres the composition of the team depends on the level of the trauma call activation. For instance, a trauma call based on mechanism may activate an ED only call, whereas a patient with deranged physiological parameters may activate a ‘full’ trauma call.
Q6. How significant is the mortality and morbidity from major trauma?
Answer and interpretation
Trauma is the leading cause of death under the age of 40 years in developed countries. It is also a major killer of older age groups, behind cardiovascular disease and cancer.
- Most victims are young males.
- There is a massive additional societal burden from morbidity affecting survivors as well.
- Most preventable deaths are due to hemorrhage.
Q7. What is the pattern of deaths from major trauma?
Answer and interpretation
Trauma deaths are classically described as having a trimodal distribution:
- immediate
- early
- late
Immediate deaths
- Seconds to minutes after injury
- Usually unpreventable eg: apnoea secondary to high spinal or brain injury, or catastrophic hemorrhage due to great vessel disruption.
Early deaths
- Minutes to hours after injury.
- Usually haemorrhage related.
- ATLS style emergency care specifically targets these patients.
Late deaths
- Days to weeks after injury.
- Usually due to multi-organ failure or sepsis.
- Optimal early management may prevent these.
As with most things that are ‘classic’, whether this schema matches reality is highly questionable (see Wyatt et al, 1995; Demetriades et al, 2005; Gunst et al, 2010)…
- Resus.ME — London trauma deaths described
- Trauma Professional’s Blog — Trauma activation patients staying too long in your ED?
Q8. What is the ‘golden hour’ of trauma care?
Answer and interpretation
The ‘golden hour’ isn’t a strictly defined time period, but is rather a concept that emphasizes the urgency of care required by major trauma patients to prevent ‘early deaths’ predominantly from haemorrhage.
- The validity of this concept remains controversial (see Lerner and Muscati, 2001).
A result of the concept is the preference for a ‘scoop and run’ approach to prehospital care — rather than “stay and play” — so that patient’s are transferred to hospital for definitive care as soon as possible. However, potentially life-saving interventions that can be provided in the field by skilled practitioners should not be delayed.
It should be noted that in a country as large as Australia, retrieval times to centres capable of providing definitive care for trauma can be prolonged (by prolonged, I mean a bloody long time! For instance, a mean of 6+ hours in the Top End of the Northern Territory).
Q9. Is trauma a “surgical disease”?
Answer and interpretation
Trauma has traditionally been considered a surgical disease, as operative intervention is regarded as definitive care. Consistent with this are American College of Surgeons (ACS) guidelines advising that a trauma surgeon be present in the ED on patient arrival, and ‘must’ be present with 15 minutes.
However, it is clear that the initial assessment and management of trauma patients can be adequately coordinated by trained healthcare professionals — such as emergency physicians — independent of specialty, as long as ready access to interventionalists is available when required. Furthermore, trauma patients are increasingly managed conservatively or there injuries are amenable to non-surgical therapies such as interventional radiology.
Also worth noting is Cliff Reid’s comment from Resus.ME:
Unfortunately for many UK and Australasian centres, the challenge that remains is not deciding when to call the surgeon, but getting one when you do call, preferable one who is not committed to an elective operating list and one who has some training and experience in trauma surgery. [Resus.ME — Surgeons and Trauma Teams]
Q10. What is a ‘seatbelt sign’?
Answer and interpretation
The seatbelt sign consists of contusions and abrasions on the abdomen of a restrained occupant involved in a motor vehicle crash. As discussed on the Trauma Professional’s Blog, this sign mandates close observation and an abdominal CT due to it’s association with intrabdominal injury (small bowel, stomach, colon) and vertebral injury (the Chance fracture) which together comprise seatbelt syndrome.

References
Journal Articles and Textbooks
- Demetriades D, Kimbrell B, Salim A, Velmahos G, Rhee P, Preston C, Gruzinski G, Chan L. Trauma deaths in a mature urban trauma system: is “trimodal” distribution a valid concept? J Am Coll Surg. 2005 Sep;201(3):343-8. PubMed PMID: 16125066.
- Fildes J, et al. Advanced Trauma Life Support Student Course Manual (8th edition), American College of Surgeons 2008.
- Gunst M, Ghaemmaghami V, Gruszecki A, Urban J, Frankel H, Shafi S. Changing epidemiology of trauma deaths leads to a bimodal distribution. Proc (Bayl Univ Med Cent). 2010 Oct;23(4):349-54. PubMed PMID: 20944754; PubMed Central PMCID: PMC2943446.
- Legome E, Shockley LW. Trauma: A Comprehensive Emergency Medicine Approach, Cambridge University Press, 2011.
- Lerner EB, Moscati RM. The golden hour: scientific fact or medical “urban legend”? Acad Emerg Med. 2001 Jul;8(7):758-60. Review. PubMed PMID: 11435197. [free fulltext pdf]
- Marx JA, Hockberger R, Walls RM. Rosen’s Emergency Medicine: Concepts and Clinical Practice (7th edition), Mosby 2009. [mdconsult.com]
- Wyatt J, Beard D, Gray A, Busuttil A, Robertson C. The time of death after trauma. BMJ. 1995 Jun 10;310(6993):1502. PubMed PMID: 7787598; PubMed Central PMCID: PMC2549879.
Social Media and Web Resources
- EMBasic Podcast — Trauma Resuscitation: Part 1 – Evaluation and Part 2 – Interventions
- The Trauma Professional’s Blog — Tips for Surgeons: Seatbelt Sign
CLINICAL CASES
Trauma Tribulation
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC

Thank you for your help and guide.
Thank you very much
Signed up to the Newsletter, GP registrar in UK going to work in A&E on my next rotation – this was very useful! Thank you