Ultrasound Case 061
Presentation
A 69 year old alcoholic patient presents with severe epigastric pain radiating through to his back. You are asked to exclude an abdominal aortic aneurysm and take a look with ultrasound.
Describe and interpret these scans
IMAGE INTERPRETATION
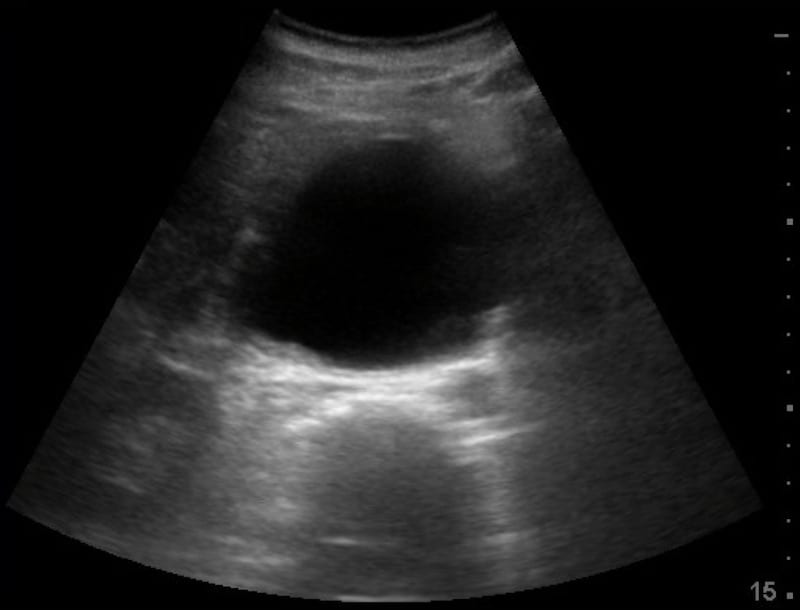
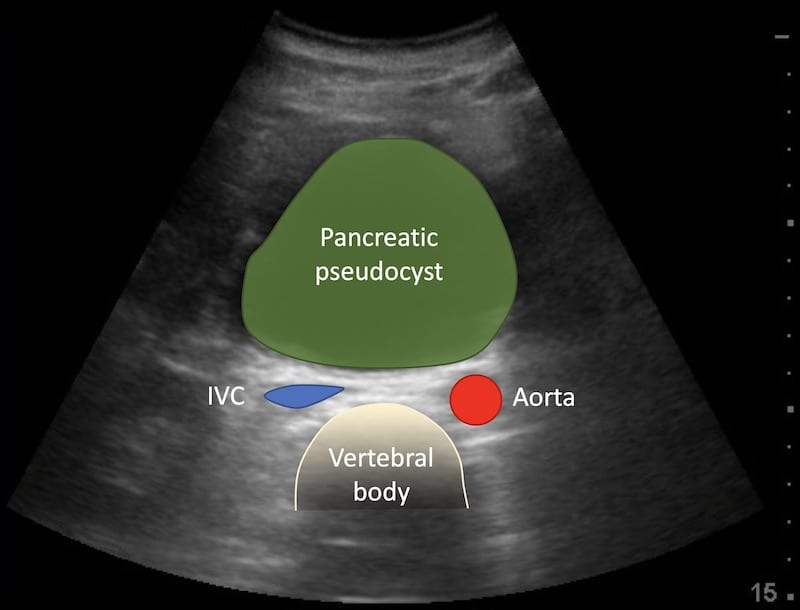
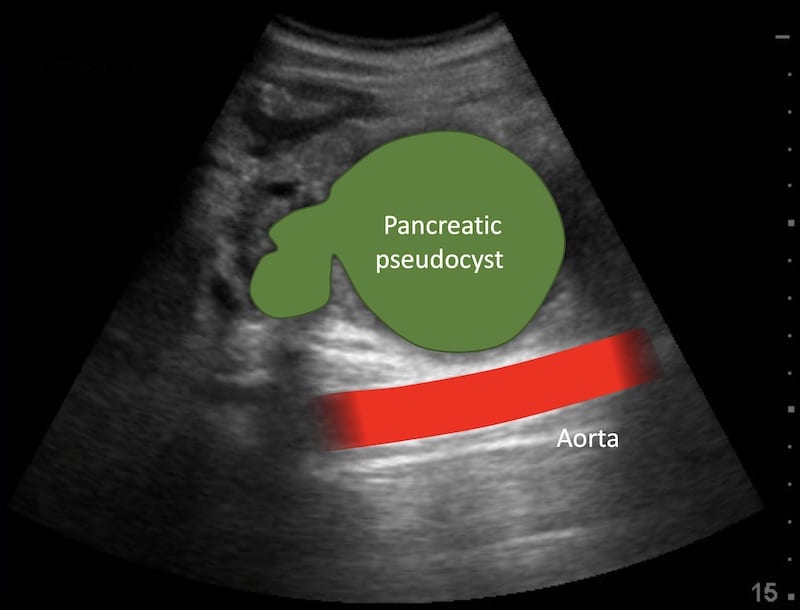
Image 1: Transverse view epigastrium. A large round hypoechoic mass is seen, it looks like an abdominal aortic aneurysm and certainly fits clinically.
Looking more carefully you can see the normal abdominal aorta behind the large cystic epigastric mass – which is a pancreatic pseudocyst.
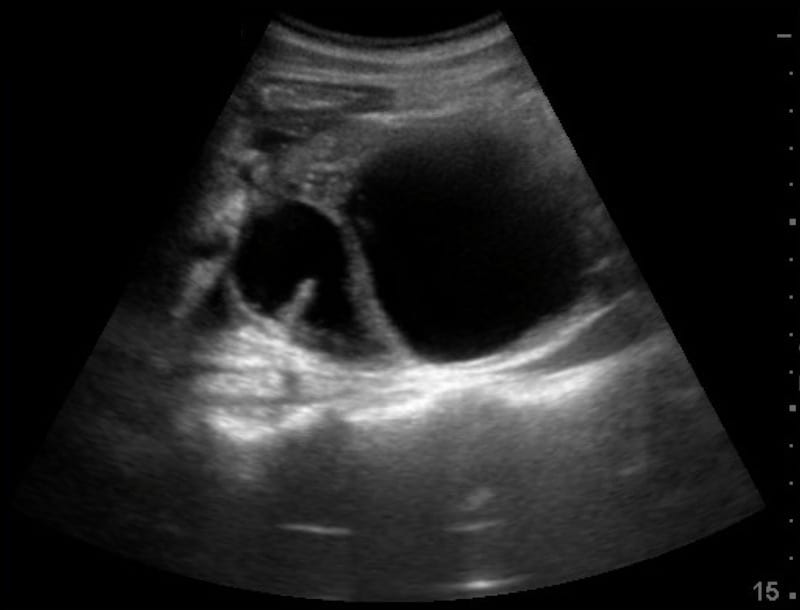
Image 2: Longitudinal view epigastrium, midline. The pancreatic pseudocyst is seen lying anterior to the vertebral bodies.
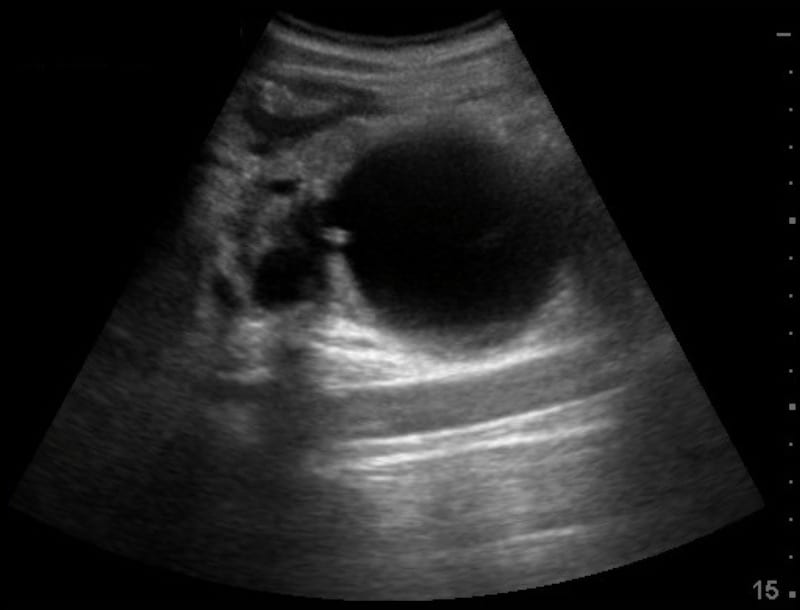
Image 3: Longitudinal view epigastrium angled to the left. The normal aorta is seen deep to the pancreatic pseudocyst. Image
CLINICAL CORRELATION
Pancreatic pseudocyst.
Pancreatic pseudocyst may masquerade as an aortic aneurysm and is a potential pitfall for the novice.
- To confirm an aortic aneurysm: Ensure your settings are optimised and orientation correct. Set your depth relatively deep – enough to ensure you are seeing the vertebral bodies. I have seen someone interpret the anterior wall of a calcified aortic aneurysm as the vertebral body, and in other cases seen them think the superior mesenteric artery and vein were the aorta and IVC respectively.
- Image it in at least 2 planes – usually transverse and longitudinal, sweeping or fanning from top to bottom in each view. Build a three dimensional picture of the structure in your mind.
- Look at the anatomical relationships particularly the vertebral body and inferior vena cava. Is what you are looking at a tubular structure?
- Hold the probe very still and look for arterial pulsations – if it pulsates in arterial fashion – the rapid expansion phase moves outwards – it is probably an artery.
- Put on colour Doppler to assess flow – but remember at greater depths flow may not be detected, flow exactly perpendicular to the ultrasound beam is not detected, slow flow may not be detected, and movement of the patient may artifactual flash colour which you may interpret as flow.
- Most importantly THINK – does this fit clinically, could it be something else?
[cite]
TOP 100 ULTRASOUND CASES
An Emergency physician based in Perth, Western Australia. Professionally my passion lies in integrating advanced diagnostic and procedural ultrasound into clinical assessment and management of the undifferentiated patient. Sharing hard fought knowledge with innovative educational techniques to ensure knowledge translation and dissemination is my goal. Family, wild coastlines, native forests, and tinkering in the shed fills the rest of my contented time. | SonoCPD | Ultrasound library | Top 100 | @thesonocave |