Vitamin D in Critical illness
OVERVIEW
Vitamin D is a fat soluble vitamin with dermal synthesis being the major natural source
- Main clinically significant role is in maintaining calcium homeostasis and bone metabolism
- There is an increasing appreciation for its pleiotropic effects, including immunomodulatory and other cellular functions
Vitamin D deficiency is common in the general population as well as the critically ill
- Severe deficiencies result in the clinical syndromes of rickets and osteomalacia
- Low levels of vitamin D have been associated with poorer outcomes in the critically ill however causality has not been proven
EFFECTS OF VITAMIN D
- Regulates calcium and bone metabolism
- Inhibiting cellular proliferation
- Inhibiting angiogenesis
- Stimulating insulin production
- Inhibiting renin production
- Modulating immune function
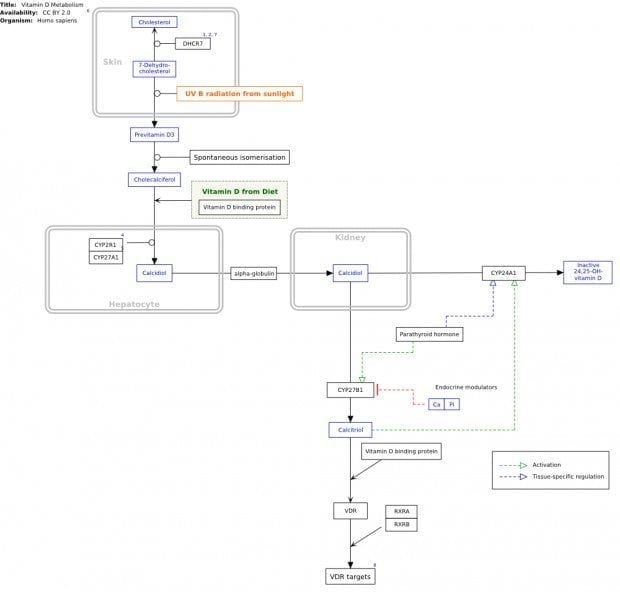
PHYSIOLOGY OF VITAMIN D
Vitamin D exists as three forms:
- Vitamin D1 (combo of ergocalciferol and lumisterol)
- Vitamin D2 (ergocalciferol)
- Vitamin D3 (cholecalciferol)
Major source is cutaneous synthesis through the effects of UV light on skin
- Cutaneous 7-dehydrocholesterol → exposed to UV light → converted to cholecalciferol in keratinocytes
- Two-step hydroxylation process occurs: liver (→ 25D aka calcidiol) then kidney (→ 1,25D aka calcitriol: active form)
Hydroxylation is under endocrine and paracrine regulation
- Calcitriol formation (renal) is simulated by PTH and hypophosphatemia → as an attempt to maintain Ca and PO4 balance
- Calcidiol formation (hepatic) is substrate-dependent (not hormonally regulated)
Most is bound to vitamin D-binding protein (88%) and albumin
- 0.03% is free only
- Serum 1,25D tightly regulated by PTH, Ca and FGF-23
MECHANISM OF PLEIOTROPIC ACTIONS
Regulation of plasma Ca and PO4 concentrations (from UTD)
- Main action of calcitriol is to enhance availability of Ca and PO4 for new bone formation and prevention of symptomatic hypoCa and hypoPO4, via
- Increased bone resorption
- Increased intestinal absorption
- Increased renal tubular Ca++ reabsorption
- Enhanced PTH-induced stimulation of bone resorption and distal reabsorption
- Regulation of hormone secretion
- Inhibits PTH synthesis / secretion
- Stimulates insulin secretion
- Stimulates FGF-23 production by osteoblasts and osteocytes (predominantly)
- Regulation of immune function
- Adaptive:
- Inhibits production of pro-inflammatory / increases production of anti-inflammatory cytokines produced by T-helper cells
- Exerts inhibitory action overall → beneficial in autoimmune disease
- Innate:
- Activates toll-like receptors in leukocytes → induction of antimicrobial peptides that kill organisms (predominantly cathelicidin)
- Cathelicidins = family of antimicrobial peptides with activity against gram-positive, gram-negative and some viruses / fungi
- Adaptive:
- Regulation of cellular proliferation and differentiation
- Stimulates cell cycle inhibitors p21 and p27 and cell adhesion molecules → may reduce cancer risk
ASSESSMENT OF VITAMIN D LEVELS
- Serum vitamin D status is assessed using 25-D levels: inactive form but stable, longer half-life
- Cut-offs for optimal vitamin D levels vary. In practice:
- > 50 nmol/L: sufficient
- 25 – 50 nmol/L: insufficient
- < 25 nmol/L: deficient
ROLE IN CRITICAL ILLNESS
Hypovitaminosis D
- Common in critical illness
- Associated with multiple diseases in ambulatory non-critically ill people
- No proven causative role in critical illness
- No trials demonstrating benefit of vitamin D supplementation in critically ill
Observational studies among critically ill
- Association between reduced 25D levels and adverse outcomes including LOS, infection, AKI and mortality
EVIDENCE
Leaf et al. Randomised controlled trial of calcitriol in severe sepsis. Am J Resp Crit Care Med, 2014; 190(5) 483 – 485
- Double-blinded RCT
- n = 67, adults with septic shock
- Single dose calcitriol (2mcg 1,25 D IV) Vs placebo
- • Results
- Calcitriol resulted in vit D level 75.5 vs placebo 16.9 at 6-hrs post dose
- No difference in plasma cytokines or hCAP-18 levels (immunological protein with inverse relation of level with susceptibility to sepsis)
- Increased expression of h-CAP mRNA, IL-10 mRNA in calcitriol group at 24 hrs
- No difference in renal injury markers
- No difference in clinical outcomes (NB but wasn’t powered to detect this)
- Conclusions
- Insufficient to warrant phase III studies
- Perhaps additional phase II studies may be warranted – do higher / repeated doses of calcitriol affect immune function?
VITdAL-ICU study, JAMA 2014
- Single-centre DB RCT, 5 ICUs
- n = 475 critically ill adult white patients with vitamin D deficiency (≤ 20ng/mL)
- Intervention: Vitamin D3 enterally Vs placebo; Vitamin D3 dose: 540,000IU load then 90,000 IU monthly for 5 months
- Outcomes
- Primary: hospital length of stay (LOS)
- Secondary: ICU LOS, percentage of 25-OH D levels higher than 30ng/mL at day 7,
- Results
- Hospital LOS: no significant difference (28.3 % 25-OH D Vs 35.3% placebo)
- Hospital and 6-month mortality: no difference
- D3 associated with better hand grip and physical performance at 6-months
- A-priori subgroup analysis of severe deficiency (≤ 12ng/mL, n = 200) found
- lower hospital mortality (28.6% [95% CI, 19.9%-38.6%]) for vitamin D3 compared with 47 deaths among 102 patients (46.1% [95% CI, 36.2%-56.2%])
- no statistically significant difference in 6-month mortality (34.7% [95% CI, 25.4%-45.0%] for vitamin D3 vs 50.0% [95% CI, 39.9%-60.1%])
- Comments and criticisms
- Strengths: well-matched at baseline, large study, selected patients with deficiency (rather than all-comers), supplemented vitamin D for a long period and long-term follow-up (6 months)
- Vitamin D supplementation led to non-significant but large difference in primary outcome, and significant improvements in physical function
- Possible mortality benefit in the group with severe deficiency is hypothesis-generating
AN APPROACH
- Hypovitaminosis D is common in the critically ill, yet has not been proven to be causative of poorer outcomes and may simply be association with increasing illness severity
- The ‘severe Vitamin D deficiency’ subgroup analysis finding of a lower in-hospital mortality with Vitamin D supplementation – that was not statistically significant at 6 months – requires further investigation
- There is currently no role for routine supplementation vitamin D in critically ill patients
References and Links
Journal articles
- Amrein K, Venkatesh B. Vitamin D and the critically ill patient. Curr Opin Clin Nutr Metab Care. 2012 Mar;15(2):188-93. doi: 10.1097/MCO.0b013e32834f0027. Review. PubMed PMID: 22186356.
- Amrein K, Schnedl C, Holl A et al. Effect of high-dose vitamin D3 on hospital length of stay in critically ill patients with vitamin D deficiency: The VITdAL-ICU Randomised Clinical Trial. JAMA 2014 Sept 20 [Epub ahead of print]. PMID: 25268295
- Holick MF. Vitamin D deficiency. N Engl J Med. 2007 Jul 19;357(3):266-81. Review. PubMed PMID: 17634462.
- Leaf DE, Raed A, Donnino MW, Ginde AA, Waikar SS. Randomized controlled trial of calcitriol in severe sepsis. Am J Respir Crit Care Med. 2014 Sep 1;190(5):533-41. doi: 10.1164/rccm.201405-0988OC. PubMed PMID: 25029202.
- Nair P, Venkatesh B. Vitamin D in the ICU: anything new under the sun? Crit Care Resusc. 2012 Dec;14(4):268-73. Review. PubMed PMID: 23230875.

Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC