Trauma! Pelvic Fractures I
aka Trauma Tribulation 027
A 27 year old female was BIBA following a horse riding accident. She arrives in the ED in spinal precautions. She had transient hypotension en route that resolved with a 500 mL bolus of normal saline. The paramedics report tenderness on palpation of her iliac crests. Her vital signs are T 36.2C, P 90/min, R 22/min, BP 115/ 70 mmHg, SpO2 98%OA and GCS 15.
As leader of the trauma team you’d better know your stuff when it comes to pelvic trauma…
Questions
Q1. Why are pelvic fractures important in major trauma?
Answer and interpretation
Pelvic fractures are important because they are associated with:
- High energy mechanisms, such as:
— motor vehicle crashes
— collisions with pedestrians
— falls from height - Major haemorrhage, which can be difficult to control
- Other major injuries
— Intra-abdominal organs (28%), including aortic injury
— Hollow viscus injury (13%)
— Rectal injury (up to 5%) - High morbidity and mortality (overall mortality is 10-30%; up to 50% if shocked)
Note that stable pelvic fractures (Tile Class A) that do not involve the pelvic ring (e.g. pubic ramus fractures and avulsion fractures) are associated with much less morbidity.
You proceed to examine the patient.
Q2. How do you examine the pelvis?
Answer and interpretation
With extreme care!
Inspect for
- echymoses, deformity, asymmetry, wounds
Palpate the skeletal structures
- pubic symphysis, iliac crests, the posterior sacroiliac joints, ischial tuberosities as well as the the spine extending inferiorly to the sacrum and coccyx
Assess for mobility
- Gently compress the iliac crests to fell for instability
- If there is no pain or movement felt on compression, gently distract the iliac crests (some experts, such as Scott Weingart, advise against distraction)
- A gentle technique and cautious approach is important to avoid aggravating haemorrhage if the pelvis is fractured.
This maneuver should only be performed once, ideally by the most senior trauma doctor present. Do not ‘rock’ the pelvis! Be gentle!
Patients with suspected pelvis fractures also need careful examination of:
- Rectum — digital rectal exam to palpate for rectal injury (e.g. blood, wounds), bony fragments, sphincter function and a boggy or high-riding prostate.
- Perineum and genitalia — check for coexistent genital trauma, blood at the meatus, and scrotal or other perineal hematomas. Perform a vaginal exam in women for vaginal tears.
- Lower limb length discrepancy and malrotation, and neurology
- The abdomen, e.g. tenderness, distention, external signs of trauma
Normal examination in an alert adult patient effectively rules out significant pelvic injury (93-100% sensitivity) unless there are distracting injuries. Any injuries missed tend to be be clinically insignificant or managed conservatively anyway.
Learn more:
- LITFL: Trauma Tribulation 026 — Trauma! Genitourinary injuries
- Trauma Professional’s Blog — What the Heck? and The Answer
Q3. Why is it important to detect rectal injury in patients with pelvic trauma?
Answer and interpretation
For these reasons:
- Rectal injury is common (up to 5%)
- signifies an open fracture — which are more likely to be hemodynamically unstable
- may require fecal diversion, pre-sacral drainage and perineal debridement
- Risk of death from secondary sepsis
As the assessment continues you consider what investigations to order.
Q4. What investigations may be useful in assessing patients with suspected pelvic fractures?
Answer and interpretation
As always investigations are selected based on history and examination to determine diagnosis, management and/or prognosis. Depending on the clinical situation additional investigations may be be needed.
Bedside tests
- Venous blood gas (VBG)
— monitor hemoglobin (Hb), lactate and acidemia in major haemorrhage - FAST scan
— assess for intraperitoneal fluid in a hemodynamically unstable patient with suspected pelvic fracture
— Positive scan suggests haemorrhage from intra-abdominal injury and the need for laparotomy
— False positives may result from associated bladder rupture - Diagnostic peritoneal aspirate (DPA)
— can be used to rule out a false negative FAST scan in a haemodynamically unstable patient
— DPA is performed above the umbilicus in patients with suspected pelvic fractures to avoid aspirating a pelvic hematoma
— A positive result is the aspiration of 10 mL of frank blood or GI contents
— this is an open procedure performed by a surgeon skilled in the technique, and may take 20 minutes
Laboratory tests
- Group and save, or cross match (4-8 units) if severely injured
- full blood count and coagulation profile
— baseline Hb to allow monitoring for a drop over time as a result of hemorrhage
— platelets and clotting factors may be depleted in major haemorrhage - BhCG in women of child bearing age
Imaging
- AP pelvis x-ray
— a normal x-ray does not exclude pelvic fractures completely, but does rule out pelvic fracture as a cause of haemodynamic instability - CT abdomen and pelvis with IV contrast
— performed in the haemodynamically stable patient to rule out intra-abdominal and retroperitoneal injury, and to characterize the type and severity of pelvic injury and may identify those suited to inetrventional radiology - Angiography
— used to identify arterial injury and to guide embolisation
Learn more:
- Resus.ME — Open book fractures and ultrasound
Q5. Which major trauma patients should get a pelvic x-ray?
Answer and interpretation
Indications for pelvis x-ray include:
- Hemodynamically unstable
- Altered mental state
- Distracting injuries
- Children (physical exam is less reliable)
- Abdominopelvic CT not being done for another reason
Do not perform pelvis x-ray if:
- Normal examination and the patient is alert and able to ambulate
- Abdominopelvic CT will be performed anyway for another reason
Note that the miss rate for pelvic fractures using plain films varies from about 4 to 23% in different studies, and other studies comparing radiographs to CT scans indicates that the sensitivity of pelvic radiographs is only 64-78%. Even when an injury is detected by plain radiography, CT is generally necessary to further delineate the nature of injury and rule out other injuries.
A CT scan is the imaging modality of choice for assessing pelvic ring injury.
Learn more:
- Trauma Professional’s blog — Pelvic Trauma Radiographs Demystified
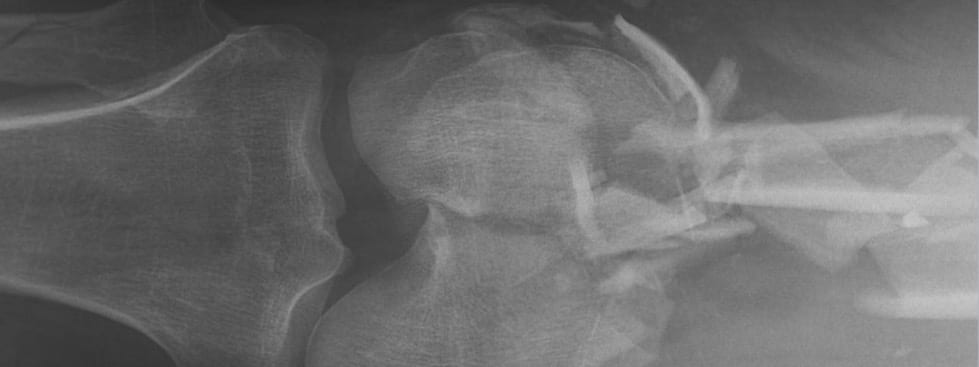
As expected the AP pelvic x-ray confirms a fractured pelvis.
Q6. How are pelvic fractures classified?
Answer and interpretation
There are various systems for classification, these are the 2 most often used:
- Tile classification
— based on pelvic stability and useful for guiding pelvic reconstruction - Young-Burgess classification
— more useful in the ED as it is based on mechanism and also indicates stability (I to III subclassification)
The Tile classification
- Tile A
— Rotationally and vertically stable
— pubic ramus fracture, iliac wing fracture, pubic stasis diastasis <2.5 cm - Tile B
— Rotationally unstable, vertically stable
B1: pubic symphysis diastasis >2.5 cm and widening of the sacroiliac joints (open book fracture due to external rotation forces on the hemipelvises)
B2: pubic symphysis overriding (internal rotation force on hemipelvises) - Tile C
— Rotationally and vertically unstable
— disruption of SI joints due to vertical shear forces
C1: unilateral
C2: bilateral
C3: involves acetabulum
The Young-Burgess classification
- Anteroposterior compression (APC)
— common feature is diastasis of the pubic symphysis or vertical fracture of the pubic rami
APC I: Pubic symphyseal diastasis, <2.5 cm, no significant posterior ring injury (stable)
APC II: Pubic symphyseal diastasis >2.5 cm, tearing of anterior sacral ligaments (rotationally unstable, vertically stable)
APC III: Hemipelvis separation with complete disruption of pubic symphysis and posterior ligament complexes (completely unstable) - Lateral compression (LC)
— common feature is a transverse fracture of the pubic rami
LC I: Posterior compression of sacroiliac (SI) joint without ligament disruption (stable)
LC II: Posterior SI ligament rupture, sacral crush injury or iliac wing fracture (rotationally unstable, vertically stable)
LC III: LC II, with open book (APC) injury to contralateral pelvis (completely unstable) - Vertical shear injuries (VS)
— common feature is a vertical fracture of the pubic rami
— displaced fractures of the anterior rami and posterior columns, including SI dislocation (completely unstable) - Combined mechanism (CM) fractures
— massive pelvic injuries that don’t fit the other categories (completely unstable)
APC fractures typically result from ‘head on’ collisions, LS fractures from ‘side on’ impacts and VS fractures from falls from height or ‘head on’ motor vehicle crashes. The Young-Burgess classification was originally thought to predict extent of haemorrhage but this has not been supported by subsequent research. The ‘lesser’ fractures can still result in arterial haemorrhage in some cases.
Q7. What other important specific injuries are associated with pelvic fractures?
Answer and interpretation
Important specific injuries associated with pelvic fractures include:
- Bladder and urethral injury (5-20%)
— posterior urethra with pelvic fractures
— anterior urethra with straddle injuries - Intra-abdominal injury
— spleen and liver (12%)
— bowel (4%) - About 5% of pelvic fractures are open and may involve rectal or vaginal tears
Other injuries (e.g. head, chest) may also be present, especially as the presence of pelvic fractures implies a high energy mechanism of injury.
Q8. What are the potential complications of pelvic fractures?
Answer and interpretation
Acute
- major haemorrhage and shock (leading mechanism of death)
- visceral and soft tissue injury:
— fractures may be compound into the perineum or vagina
— lacerations into the rectum or bladder
— urethral injuries common in males - sacral plexus injury
- ileus
- fat embolization
- acute respiratory distress syndrome
- venous thromboembolism
- abdominal compartment syndrome
Late
- infection (second most common mechanism of death)
- fracture complications (e.g. osteoarthritis, malunion)
- disability and immobility
- incontinence
- sexual dysfunction
- dystocia following subsequent pregnancy
The management of pelvic trauma and ensuing hemorrhage is discussed in Trauma Tribulation 028 — Trauma! Pelvic Fractures II.
References
LITFL
- Weingart on Pelvic Trauma
- Pelvic and Hip injuries in the Emergency Department
- Trauma Tribulation 026 — Trauma! Genitourinary injuries
Journal articles and textbooks
- Cullinane DC, Schiller HJ, Zielinski MD, Bilaniuk JW, Collier BR, Como J, Holevar M, Sabater EA, Sems SA, Vassy WM, Wynne JL. Eastern Association for the Surgery of Trauma practice management guidelines for hemorrhage in pelvic fracture–update and systematic review. J Trauma. 2011 Dec;71(6):1850-68. Review. PubMed PMID: 22182895.
- Fildes J, et al. Advanced Trauma Life Support Student Course Manual (8th edition), American College of Surgeons 2008.
- Legome E, Shockley LW. Trauma: A Comprehensive Emergency Medicine Approach, Cambridge University Press, 2011.
- Marx JA, Hockberger R, Walls RM. Rosen’s Emergency Medicine: Concepts and Clinical Practice (7th edition), Mosby 2009. [mdconsult.com]
- Suzuki T, Smith WR, Moore EE. Pelvic packing or angiography: competitive or complementary? Injury. 2009 Apr;40(4):343-53. Epub 2009 Mar 17. Review. PubMed PMID: 19278678.
- White CE, Hsu JR, Holcomb JB. Haemodynamically unstable pelvic fractures. Injury. 2009 Oct;40(10):1023-30. Epub 2009 Apr 16. Review. PubMed PMID: 19371871.
Social media and other web resources
- EMCrit — Severe Pelvic Trauma
- EMRAP November 2006 — Carlos Brown: Pelvic Exsanguination (subscription required)
- Free Emergency Medicine Talks — Thomas Scalea 2010: Pelvic Trauma
- Free Emergency Medicine Talks — Julie Gorchynski 2011: Stabilizing Pelvic Fractures: Is Anything New?
- Free Emergency Medicine Talks — Sachin Shah 2010: Pelvic Fractures
CLINICAL CASES
Trauma Tribulation
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
