Stroke Infarction: Clot Retrieval
Endovascular clot retrieval (ECR) is a highly effective treatment for restoring cerebral blood flow in eligible patients with ischaemic stroke.
ECR is a time-critical and technically specialised procedure
- Early intervention is crucial for optimal outcomes.
- ECR requires well-coordinated systems to identify and transport candidates to an ECR-capable centre.
- Performed by experienced neurointerventionists—radiologists, neurologists, or neurosurgeons—at select tertiary centres.
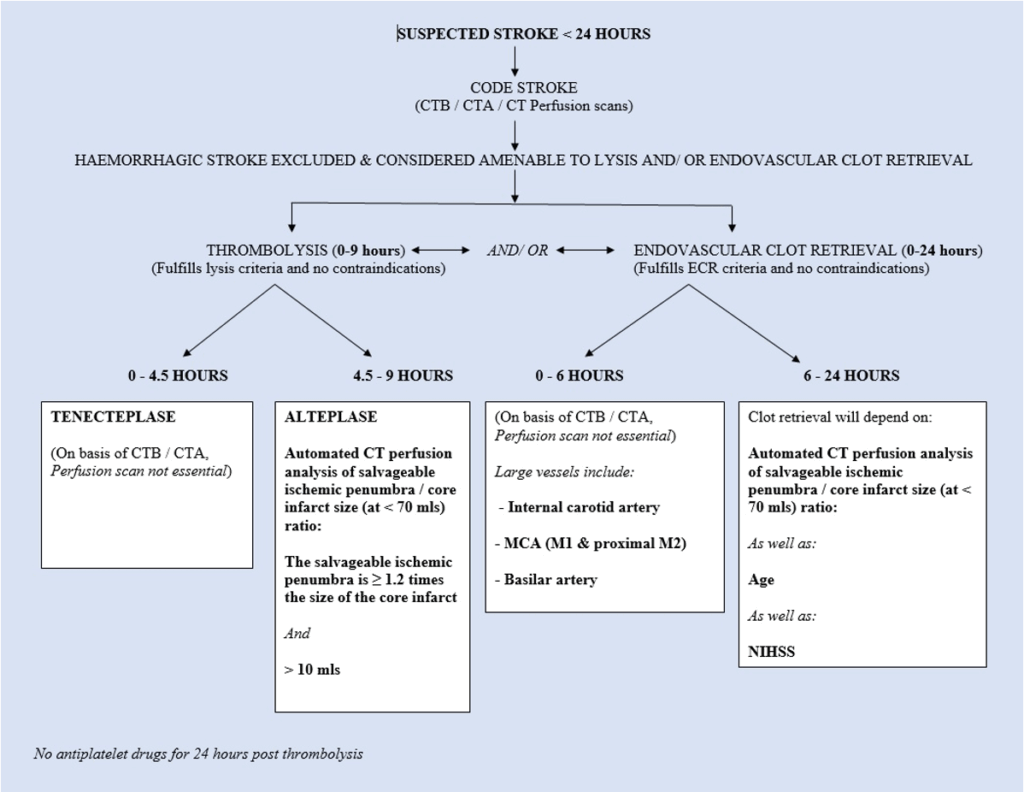
- Patients may be eligible up to 6 hours from symptom onset, or up to 24 hours in selected cases (e.g. ischaemic penumbra or basilar artery stroke).
Pathophysiology
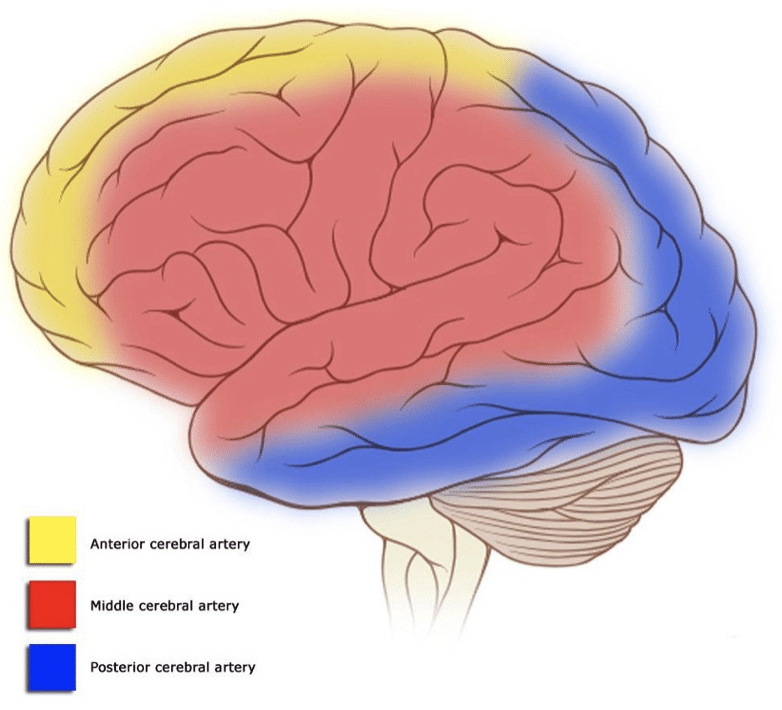
- Most strokes (≈80%) are ischaemic, caused by arterial occlusion.
- Intravenous thrombolysis is effective for smaller clots but often insufficient for large vessel occlusions.
- ECR involves intra-arterial removal of the thrombus, often in combination with thrombolysis.
- Up to 70% of patients benefit if treated within the appropriate time window.
Indications
Eligibility criteria:
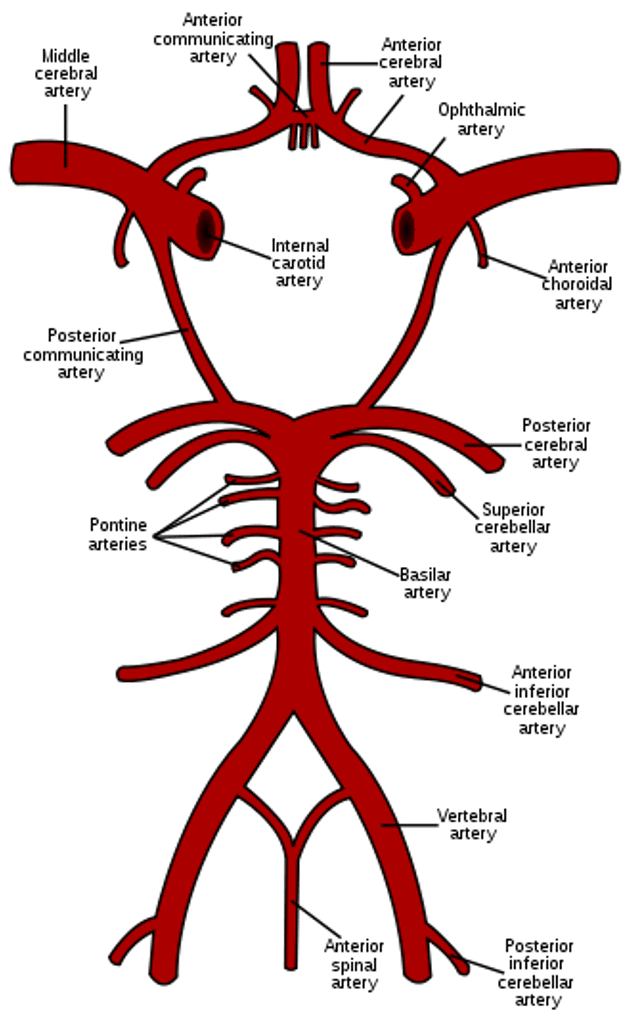
- Ischaemic stroke with confirmed large vessel occlusion on CTA:
- Internal carotid artery (ICA)
- Middle cerebral artery (MCA):
- M1 segment (carotid terminus to MCA bifurcation)
- Early M2 segment (within Sylvian fissure)
- Basilar artery
- Premorbid independence (Modified Rankin Score 0–2)
- Time of presentation:
- Within 6 hours of onset
- 6–24 hours if:
- Clinical–radiological mismatch (NIHSS vs infarct volume)
- Large ischaemic penumbra on CTP or MRI
- Basilar artery occlusion with high risk of morbidity/mortality
- Intravenous thrombolysis initiated (if eligible and within 4.5 hours)
- Access for clot retrieval, as confirmed by a neurointerventionist (e.g. via PACS)
Clinical assessment
- <4.5 hours → Thrombolysis candidate
- <6 hours (large vessel occlusion) → Thrombolysis + ECR
- 6–24 hours (selected patients) → ECR considered
Investigations
Blood tests:
- FBC
- U&Es / glucose
- Coagulation profile
- CRP / ESR
ECG:
- Assess for atrial fibrillation
Imaging:
- Non-contrast CT:
- Haemorrhage, infarction, stroke mimics, early changes, hyperdense thrombus
- CT angiography (CTA):
- 4-vessel scan (aortic arch to vertex)
- Identifies:
- Occlusions
- Carotid/proximal stenosis
- Underlying AVMs
- “Spot sign” in ICH
- CT perfusion (CTP):
- Confirms:
- Large vessel occlusion
- Viable penumbra
- Extent of infarct core
- Confirms:
If imaging uncertainty exists, consult stroke team immediately.
Management
Pre-hospital
- Transport to thrombolysis-capable centre within 60 minutes
- Pre-notify ED with patient details and stroke onset time
ED thrombolysis
- Eligible patients receive IV tPA
- If suitable for ECR, prepare for inter-hospital transfer
Systems protocols
Key components:
- Ambulance pre-notification
- Code Stroke activation in ED
- Direct-to-CT scan access
- Stroke–neurointerventionist liaison
- Rapid ambulance transfer to 24/7 ECR centre
Airway preparation
Routine intubation not needed for anterior stroke transport.
Indications for intubation (e.g. basilar stroke or ICH):
- Low GCS (not due to aphasia)
- Agitation
- Respiratory compromise
- Haemodynamic instability
Endovascular clot retrieval
- Requires rapid assessment, team coordination, and advanced skills.
- Best outcomes occur with early flow restoration.
- Performed only at specialist centres.
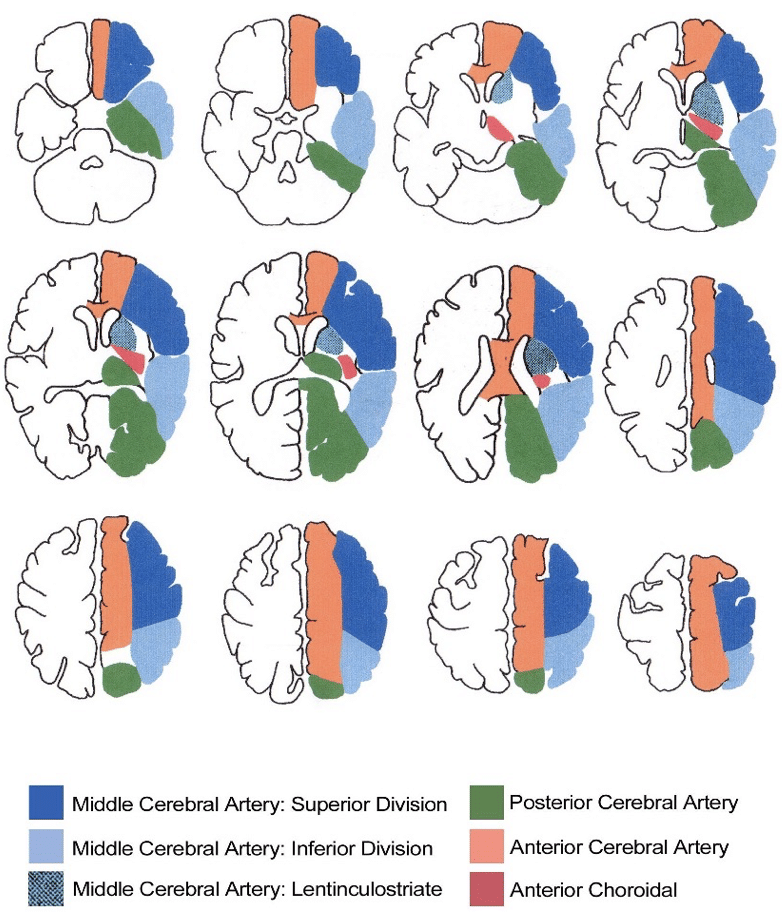
Appendix 1
Appendix 2
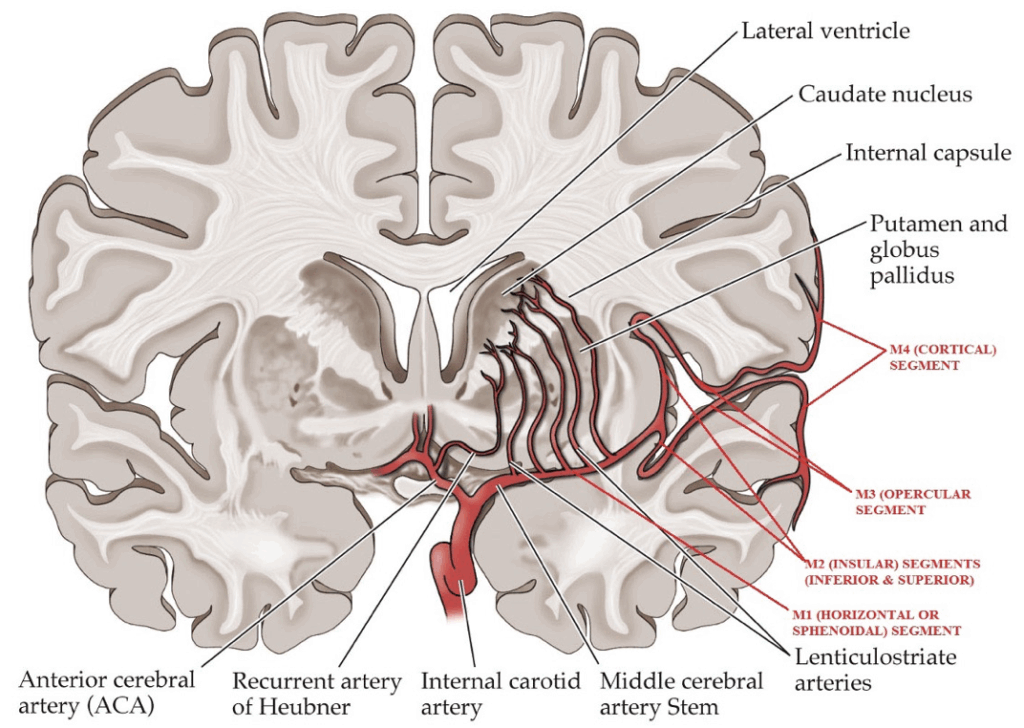
Note that the MCA segments should be thought of more as progressive generational branchings (with consequent increase in numbers of branches with each generation), rather than as strict single linear anatomical extensions.
The four radiological segments of the Middle Cerebral Artery are as follows:
M1: The horizontal (or sphenoidal) segment:
- This segment arises from ICA and travels in lateral direction, parallel to the sphenoid wing and terminates by dividing into the M2 segments.
- The MCA bifurcates in approximately 70% of cases, trifurcates in 20% of cases and divides into four branches in 10% of cases.
- Branches include:
- The lenticulostriate perforating vessels
- Anterior temporal artery.
M2: The insular segments:
- Most commonly there are two of these – an inferior and a superior division.
- They extend from the end division point of the M1 segment, and run to the circular sulcus of insula where they make hairpin bend to continue on as the M3 segments.
- The insular segments run over the insula within the Sylvian fissure and terminate at the circular sulcus of the insula.
M3: The opercular segments:
- The opercular segments, begin at the circular sulcus of the insula and run within the Sylvian fissure to terminate at the surface of the fissure.
M4: The cortical segments:
- The cortical branches begin at the surface of the sylvian fissure and extend over the convex surface of the cerebral hemispheres.
- These cortical branches can also be grouped according to which M2 segment they arise from as follows:
- Superior division: Orbitofrontal, prefrontal, precentral, and central arteries.
- Inferior division: Temporo-polar, temporo-occipital, angular, and anterior, middle, and posterior temporal arteries.
- Dominant division: These branches can arise from either division, and usually come off the larger of the MCA divisions). Anterior and posterior parietal arteries.
Appendix 3
Appendix 4
Appendix 5
References
Publications
- Nogueira RG et al; DAWN Trial Investigators. Thrombectomy 6 to 24 Hours after Stroke with a Mismatch between Deficit and Infarct. N Engl J Med. 2018 Jan 4;378(1):11-21.
- Tremonti C, Thieben M. Drugs in secondary stroke prevention. Aust Prescr. 2021 Jun;44(3):85-90.
- Clinical Guidelines for Acute Stroke Management – National Stroke Foundation
- Brazis PW, Masdeu JC, Biller J. Localization in Clinical Neurology. 8e 2021
- Fuller G. Neurological Examination Made Easy. 6e 2019
- O’Brien M. Aids to the Examination of the Peripheral Nervous System. 6e 2023
FOAMed
- Flower O. Clot retrieval for stroke. LITFL
- Flower O. Old Brain, New tricks. LITFL
- Davidson J. CT Case 061. LITFL
- Beech G. CT Case 083. LITFL
- Coni R. Neuro 101: Cerebral Hemispheres. LITFL
- Nickson C. Stroke Thrombolysis. LITFL
Fellowship Notes
MBBS DDU (Emergency) CCPU. Adult/Paediatric Emergency Medicine Advanced Trainee in Melbourne, Australia. Special interests in diagnostic and procedural ultrasound, medical education, and ECG interpretation. Co-creator of the LITFL ECG Library. Twitter: @rob_buttner
Educator, magister, munus exemplar, dicata in agro subitis medicina et discrimine cura | FFS |


