A Mortal Battle with Four Hour Medicine
aka To Err is human 003
A Post in 2 parts…
Act I: The Existential Installment.
Act II: The Clinical Section.
WITH a cliffhanger.
The Scene
The heartland of the four hour rule, a tertiary emergency department trauma centre, showcased the world over for its early and aggressive adoption of the four hour target, where overseers donning clipboards are omnipresent, moderately feared and powerful.
It is 2330h on a weeknight, and the ED is slopping at the sides it is so full. There is a constant drone of noise and action, in an attempt to get the occupants out of the department, either to a ward, or to their own dwellings. All avenues are explored to fulfill this utopic vision of numeric and data driven perfection. The resuscitation area is stuffed full of people in various stages of dying, either heading towards the end, or being dramatically clawed back.
Out the back, in the unfashionable part of the throbbing metropolis, lies a young, previously fit and well woman, who is surprisingly, well, normal (for this psychotic part of the world anyway). She has been waiting, uncomplaining, for over 3 hours, with a minor complaint of 6 days of vomiting.
The Players
The Patient:
Sitting up, sipping water. Returned 3 days ago from a trip to Thailand. She is 33 years old, works in accounts, is fit and healthy, partakes in no illicit drugs or alcohol, is not sexually active, and had only been in Thailand for 4 days prior to her starting vomiting. She was perfectly fine before this.
The Junior Doctor:
He has seen the patient and gives a seemingly perfectly plausible history – prefaced with a presumptive diagnosis of gastroenteritis. Worsening onset of nausea and vomiting. No diarrhea. No fevers. No companions with similar. No urinary symptoms. He thinks she looks quite well, has popped in a line, given her some metoclopramide, and is happy that she has had symptomatic improvement, and would now like to send her home, as the feared clipboards are coming at him. He hasn’t sent bloods, because he has had it drummed into him that we over-order bloods, and cause unnecessary cost and delay.
The Senior Consultant:
Having been at work since 0900, addled brain somewhat fried by a long shift of teaching, trauma and trouble, due to finish at 2400, very happy to hear such a simple scenario, to tidy up the final moments of shift. Considers just signing off on the story alone, but decades of work in the same dept suggest that she should actually eyeball the patient.
The Action
No twist at this point – true enough, the patient is sitting up, sipping water. Does look a little pale, a little wan. But, in truth, there is not much more to the story. No high risk activities, no contacts, no other specific symptoms on systemic enquiry. But her face does look a little puffy. The dialogue reveals on closer questioning that yes, she had noticed that, but hadn’t really thought too much of it. No, her ankles hadn’t swollen up, but yes, her rings might have been a little tight.. No, she wasn’t at all short of breath. She has had some mild generalized abdominal pain, for which she saw her GP 2 days ago, who prescribed ibuprofen, and augmentin duo forte.
At this point a nebulous primordial soup of potential errors swirls around this little corner. The words of Patrick Croskerry echo silently through the leaden cognitive steps being taken. How many potential errors had the possibility to occur at this moment?
Anchoring Bias: The tendency to be influenced by features encountered early in the presentation of the illness, often committing to a premature diagnosis. On the triage sheet alone – ‘just back from Thailand. Vomiting’ may be enough for a rapid diagnosis to be pounced upon.
Confirmation Bias: The tendency to search out or interpret information that appears to confirm a diagnosis, giving less weight to data that might disprove a theory. In this case, a normal set of vital signs and a not unwell looking woman all confirmed the resident’s idea that this was a simple illness. No other data was sought
Clustering Bias: The tendency to see patterns where none actually exist. This RMO had already seen a mild case of gastroenteritis earlier that evening
Search Satisficing: Where the physician calls off the search for further abnormalities having achieved satisfaction from finding the first – perhaps a reason for labs not being taken
Then there is the influence of ambient conditions: This particular situation was heaving with some of these operating characteristics listed below, but you put together a high decision density environment, with (extreme) time pressures, constant interruptions and junior doctor inexperience and you have a veritable perfect recipe for error.
Unique operating characteristics of the emergency department predisposing to medical error:
- High levels of diagnostic uncertainty
- High decision density
- High cognitive load
- High levels of activity
- Inexperience of some physicians and nurses
- Interruptions and distractions
- Uneven and abbreviated care
- Narrow time windows
- Shift work
- Shift changes
- Compromised teamwork
- Poor feedback
At this point the deep, dark, but always respected, little alarm bell unhappily (at 2345h) rings away. The RMO is brought back bedside, and bloods and ECG are requested, whilst further history is dragged out.
How much had she vomited? Well she had trouble getting her head out of the toilet bowl all day today. When asked to produce a urine, she said she’d certainly try, but she was not sure that she could. When did you last pass urine? Maybe a couple of days ago, was the response.
Stop! What was that?
The Cliffhanger
Fairly rapidly, the labs are obtained.
Here are the electrolytes:
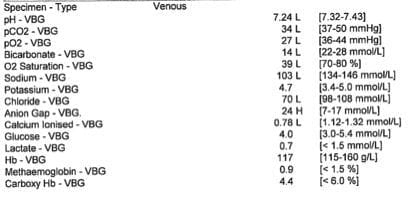
Jolted into action (and rather concerned about the lack of K+ on the sample – ‘haemolysed!’ Pah.), the urgency for ECG is stated (plum normal), and a VBG to look for K+ and acid/base variables.
The VBG:
At this point the clinical discussion will be opened up to the wondrous world of LITFL blog readers.
- What is going on?
- What additional information do you need to further the diagnostic and management journey?
The Last Word
Metacognition.
I put this in for two reasons. One, because Seth Trueger newly graduated F.UCEM (aka @mdaware) loves any word that is prefixed with meta-, the other being is that it describes the process by which we reflect upon and have the option of regulating our thinking. Being aware of how and why we make errors is the first step into avoiding making them.
Burgeoning work is going on in reducing errors in the ED, including checklists, and education into cognitive biases. Much is made from the comparison between our own and the aviation industry. I, for one, however, do not like this comparison – how can you compare the infinite complexity of the human presentation with a machine? A pilot does not, on the whole, get into his plane, and all of a sudden discover it is a car, whereas the equivalent in emergency medicine is quite common. Having said that, there is much that can be LEARNT from that industry.
There is much opinion I could post on the influence of time targets (as anyone with the misfortune of being within earshot of me could attest), however I shall stick with the point that aggressive time targets and interruptions are acknowledged as contributing to error. We should be wary of introducing new policies and practices that actively increase errors, rather than trying to reduce them.
And the REAL last word goes to the eloquent Dr Croskerry:
“We do not make good decisions when our viscera are aroused”
References
- The Doct-Aviator
- To Err is Human 001 — Are you Satisficed?
- To Err is Human 002 — Entrapped
- Bleetman A, Sanusi S, Dale T, Brace S. Human factors and error prevention in emergency medicine. Emerg Med J. 2012 May;29(5):389-93. Epub 2011 May 12. PMID: 21565880.
- Carley, S. Highlights from this Issue. Emerg Med J 2012;29:5 347
- Croskerry P. The cognitive imperative: thinking about how we think. Acad Emerg Med. 2000 Nov;7(11):1223-31.[PMID 11073470]
- Croskerry P, Sinclair D. Emergency medicine: A practice prone to error? CJEM. 2001 Oct;3(4):271-6. [PMID 17610769]
…Act II, and an epilogue, await

CLINICAL CASES
to err is human
Emergency physician. Lives for teaching and loves clinical work, but with social media, she is like the syndromic cousin in the corner who gets brought out and patted on the head once in a while | Literary Medicine | @eleytherius | Website |


It is always a bit embarassing to think of very rare disease – am I just trying to be clever? but for me there are 2 clues: the very well tolerated severe hyponatremia and a very low ca level in metabolic acidosis. I beliebte it is not uncommon for Addison disase to be diagnosed when decompensated by water and electrolyte loss by gastronrteritis. A combining answer to all facto would be autoimmune polyendocrine syndrom with Addison and hypoparathroidism. Renal tubalar dsyfunction is a Differential.