A Problem with Plumbing
aka Unusual Urine 006
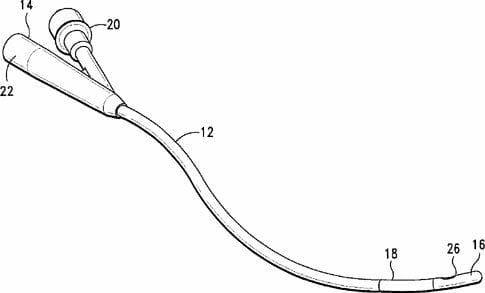
A 62 year-old male presents to the emergency department with a problem with his plumbing. Last week he had an indwelling catheter inserted for urinary retention. He was to have a trial of void today, but the Continence Nurse hasn’t been able to remove the indwelling catheter (IDC, aka Foley catheter). It seems that the balloon won’t deflate.
What are you going to do?
Questions
Q1. What is the first thing to do when confronted with this problem?
Answer and interpretation
Inspect all visible parts of the catheter to try to identify any likely sites of obstruction.
Usually the problem affects parts of the catheter inside the patient.

You’ve done that, but are none the wiser.
Q2. What will you do next?
Answer and interpretation
Sometimes IDCs cannot be removed because of ‘cuffing‘.
Cuffing usually occurs when the balloon is deflated rapidly, such that it deflates asymmetrically and doesn’t fully deflate. This means that it can snag at the bladder outlet when removal is attempted.
The first step should be to reinflate the balloon with 1 mL of saline, then slowly deflate it again. Make sure the balloon is in the bladder — not the urethra — before inflating!
This may overcome the ‘cuffing’ problem and facilitate removal.
You tried that. It didn’t work. Now what?
Q3. What are the most common causes of balloon deflation failure?
Answer and interpretation
Failure of balloon deflation prevents removal of the IDC. This is most commonly caused by:
- debris in the inflation/deflation channel (crystals may form inside the balloon or the channel to which it is attached).
- malfunction of the valve in the inflation/deflation channel.
Checking that the IDC balloon inflates and deflates correctly prior to insertion does not remove the risk of later problems.
If you have ultrasound available, confirm that the IDC balloon is inflated — in patients with prolonged catheterisation concretions may form around the catheter tip. Forceful removal may result in an inadvertent TURP!
- Ultrasound Top 100 – Case 042
Q4. What are your next steps in trying to remove the IDC?
Answer and interpretation
Attempt to disrupt the inflation/ deflation channel.
This can be done in a step-wise manner:
- cut off the inflation port syringe adaptor plug. This will allow removal of the IDC if the syringe adaptor plug is the source of the problem. It is not usually effective. There may be a defect further down the channel, so cutting further along the IDC may remove the defect… but don’t cut too low — just on the patient’s side of a suspected obstruction — and clamp the catheter with forceps to prevent recoil into the urethra. You don’t want to lose the remaining part of the IDC somewhere inside!
- attempt to aspirate fluid from the inflation/ deflation channel and collapse the balloon.
- if the above have failed, insert a thin rigid wire (e.g. central line guidewire) into the channel. This may overcome the valve-flap defect. If not the wire may be used to puncture the balloon by advancing all the way along the inflation/ deflation channel.
Some suggest injecting contrast into the inflation/ deflation channel to determine the level of obstruction. Also, some suggest that cutting the catheter should be performed only as a last resort — in which case, you might prefer to attempt the methods described in Q4 prior to cutting the catheter.
You tried those steps too. Still no luck.
Q5. What is your next approach to removing the IDC?
Answer and interpretation
Attempt to puncture the balloon with a needle.
Needle puncture of the balloon can be attempted as follows:
- over inflate the balloon (50-100 mL of saline)
- apply gentle traction to stabilize the IDC balloon against the bladder neck.
- Use a 25 Fr spinal needle (under local anesthesia) to attempt percutaneous balloon puncture. This may be performed blindly, but is best performed under ultrasound guidance.
- An alternative approach in females is to gentle advance the needle up the urethra alongside the IDC to attempt balloon puncture (transurethral approach).
Transrectal and transvaginal approaches to balloon puncture are also options.
Q6. What if you are still unsuccessful?
Answer and interpretation
It’s time to call a urologist!
If the previous methods are unsuccessful, it is best to seek advice from a urologist. Other balloon rupture techniques may be tried, but chances are the patient will require cystoscopy.
Q7. What other methods of IDC balloon rupture are there?
Answer and interpretation
There are at least two other methods:
- balloon erosion by instilling a volatile or corrosive substance
- overfilling the balloon with saline
These methods may lead to fragmentation of the IDC balloon, or in the latter case, painful bladder distention.
Instillation of volatile or corrosive substances such as toluene, ether, acetone or mineral oil may achieve balloon rupture. One technique described in Roberts and Hedges is the installation of 10 mL of mineral oil down the inflation/ deflation channel and into the balloon. If success is not achieved after 10 minutes a further 10 mL may be administered.
Alternatively, the balloon may be ruptured by overfilling with saline. This may require as much as 200-300 mL of saline administered into the balloon. The bladder itself should be filled with 100 mL of saline first, to cushion the effects of balloon rupture.
Q8. What are the complications of balloon deflation techniques?
Answer and interpretation
Complications include:
- injury to local structures, such as needle puncture of the rectum during attempted balloon perforation —
rectal puncture is generally of negligible clinical significance. - balloon fragmentation —
this may lead to foreign body stone formation. The methods described in Q6 are at high risk of causing this complication. If fragmentation is suspected the patient should undergo cystoscopy. - chemical cystitis —
this is a complication of the instillation of erosive substances as described in Q6. If these methods are used (not recommended), the bladder should be copiously irrigated withe saline following replacement of the IDC.
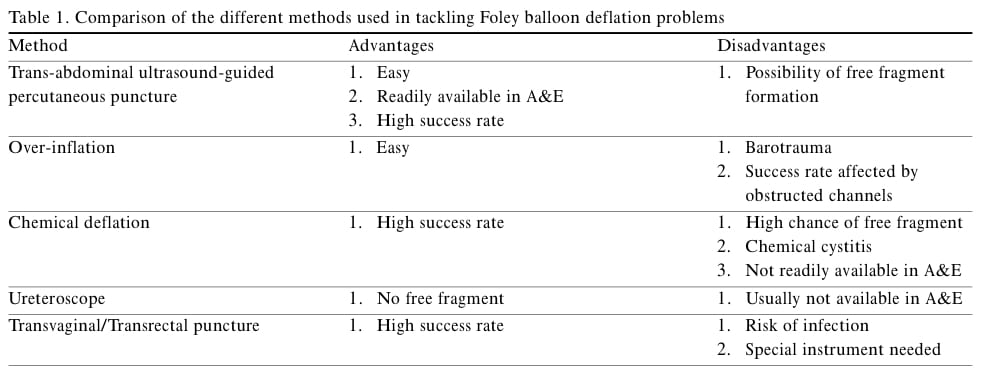
The pros and cons of different methods are shown in this table from Lee et al, 2005:
Q9. What should be done following removal of the malfunctioning IDC?
Answer and interpretation
The IDC must be inspected for missing fragments.
If missing fragments are suspected the patient will require cystoscopy so that they may be found and removed. If there are no fragments missing, the IDC can be replaced as indicated.
References
- Ultrasound Top 100 – Case 027 (Blood clot in the bladder with IDC in place)
- Ultrasound Top 100 – Case 041 (Misplaced urinary catheter)
- Ultrasound Top 100 – Case 042 (Urinary catheter balloon being inflated)
- Lee WMM, Tsui KL, Kam CW. Trans-abdominal ultrasound-guided suprapubic puncture of a non-deflating Foley catheter balloon Hong Kong J Emerg Med. 2005;12:42-45
- Patterson R, Little B, Tolan J, Sweeney C. How to manage a urinary catheter balloon that will not deflate. Int Urol Nephrol. 2006;38(1):57-61
Unusual Urine
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC