Amisulpride toxicity
Amisulpride is an atypical antipsychotic in low doses will causes and anticholinergic effect but at higher doses prolongs the QT interval with cases of torsades de pointes noted.
Toxic Mechanism:
Dopamine antagonist (D2 and D3) with some affinity for serotonin, histamine and muscarinic receptors.
Toxicokinetics:
- Oral bioavailability of 50%
- 2 absorption peaks, 1 hour and 4 hours, may occur later in overdose
- Large volume of distribution 5.8 L/kg
- Excreted unchanged in the faeces and urine
- Elimination half life 12 hours
Resuscitation:
- CNS depression (even GCS 12) requires prompt intubation and ventilation
- Hypotension:
- 20ml/kg crystalloid bolus, sodium bicarbonate 2 mmol/kg may restore a MAP >65.
- Failing this adrenaline and noradrenaline infusions can be used (peripherally at first until able to insert a central line when higher doses can be used, of note the risks of extravasation i.e. tissue necrosis is the same as for push dose pressures and using meteraminol/aramine. Make sure you have a big flowing peripheral line).
- Noradrenaline dose: 0.15mg/kg in 50ml D5W at 1-10ml/hr (0.05 – 0.5 mcg/kg/min).
- Adrenaline dose: 0.15mg/kg in 50ml D5W at 1-10ml/hr (0.05 – 0.5 mcg/kg/min).
- Bradycardia:
- Atropine 0.01 – 0.03 mg/kg IV (temporising)
- Isoprenaline 1 – 10 micrograms/min IV infusion (0.05-1.0 microgram/kg/min in children)
- Adrenaline infusion
- Torsades de pointes:
- Administer magnesium sulfate 10 mmol (0.05 mmol/kg in children) IV over 15 minutes.
- Correct hypoxia, hypokalaemia and hypocalcaemia
- If heart rate is <100 beats/minute commence an isoprenaline infusion IV at 1-10 microgram/min (0.05-1.0 microgram/kg/min in children) or overdrive pacing to maintain heart rate at 100-120 beats/minute.
Risk Assessment
- Small overdoses (<4 grams) may cause mild sedation and mild anticholinergic features. Rarely QT prolongation and torsades de pointes have been reported in this dose range
- >4 grams results in increasing risk of bradycardia, hypotension, QT prolongation, torsades de pointes and CNS depression. Coma and seizures have occurred in large overdoses.
- Remember bradycardia increases the risk of torsades de pointes in the poisoned patient
- Children: Any ingestion requires investigation
Supportive Care
- If hypotensive or bradycardic, invasive monitoring and central access maybe required.
- If intubated see FASTHUGSINBED for further supportive care.
Investigations
- Screening: 12 lead ECG, BSL, Paracetamol level
- Specific:
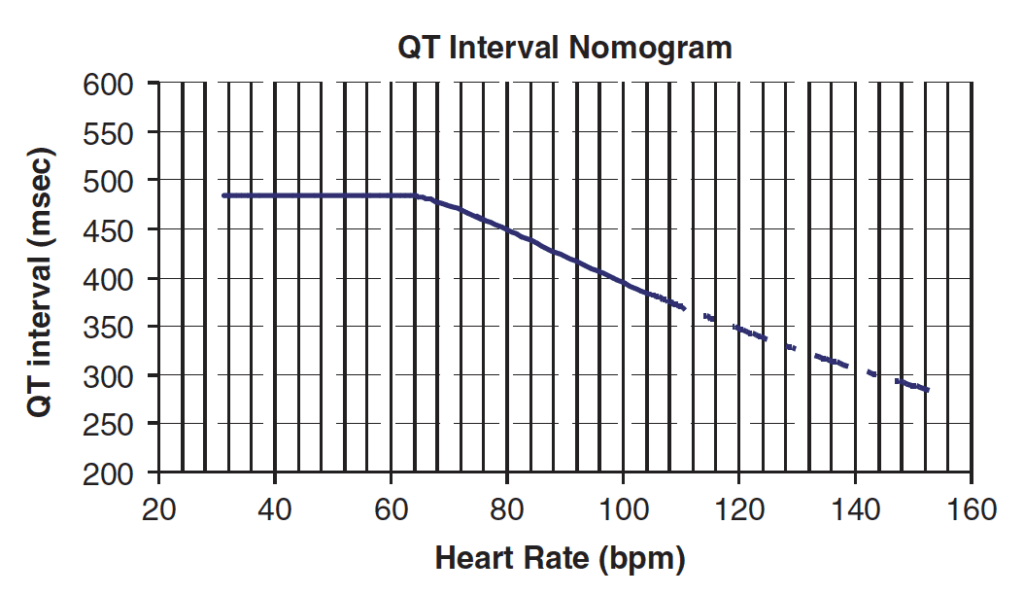
- Serial ECGs, if there is any QT prolongation then the patient requires continuous cardiac monitoring until the QT is normalised.
- ECG monitoring is required for a minimum of 16 hours if the dose exceeds 4 grams
- EUC, Mg and Ca levels
Decontamination:
- 50g of activated charcoal maybe given to the alert and cooperative patient who has ingested > 4 grams within the previous 4 hours.
Enhanced Elimination
- Not clinical useful
Antidote
- None available
Disposition
- Patients who are asymptomatic and have a normal ECG at 4 hours are medically cleared
- Patients who have ingested >4 grams and are asymptomatic and have a normal ECG at 16 hours are medically cleared
- Symptoms or QT prolongation require continued cardiac monitoring until resolution
- Patients with cardiac instability or those who are intubated require admission to HDU or ICU.
References and Additional Resources
Additional Resources:
- CCC – ECG in toxicology
- ECG Library – Polymorphic VT and Torsades de Pointes
References:
- Isbister GK, Balit CR, MacLeod D, Duffel SB. Amisulpride overdose is frequently associated with QT prolongation and torsades de pointes. Journal of Clinical Pharmacology 2010; 30:391-395
- Isbister GK, Murray L, John S et al. Amisulpride deliberate self poisoning causing severe cardiac toxicity including QT prolongation and torsades de pointes. Medcical Journal of Australia 2006; 184:354-356
- Murray L et al. Toxicology Handbook 3rd Edition. Elsevier Australia 2015. ISBN 9780729542241

Toxicology Library
DRUGS and TOXICANTS
Dr Neil Long BMBS FACEM FRCEM FRCPC. Emergency Physician at Kelowna hospital, British Columbia. Loves the misery of alpine climbing and working in austere environments (namely tertiary trauma centres). Supporter of FOAMed, lifelong education and trying to find that elusive peak performance.