Axillary and subclavian vein thrombosis
Axillary and subclavian vein thrombosis is an important diagnosis to make. The incidence of pulmonary embolism (PE) and long-term sequelae is high in untreated cases. It is associated with PE in 6–30% of cases and therefore requires anticoagulation.
Thrombosis can be primary (Paget-Schroetter syndrome / effort thrombosis / spontaneous upper extremity venous thrombosis) or secondary to identifiable causes.
Routine anticoagulation is recommended in all cases. For young, fit patients, specialist advice regarding thrombolysis, imaging, and surgery may significantly improve outcomes. Early referral to vascular surgery is recommended when the cause is uncertain.
History
- Paget-Schroetter syndrome was first described by Sir James Paget (1875) and later by Leopold Von Schrötter (1884).
- Paget-Schroetter syndrome and also known as “effort” or “spontaneous” upper extremity venous thrombosis.
Epidemiology
Incidence has increased due to catheter use in patients with cancer and chronic conditions.
Pathophysiology
Causes
1. Primary / Spontaneous Thrombosis:
- Often effort-induced in predisposed individuals
- Strenuous effort with the arm in the overhead or hyper-abducted position is thought to be a risk factor, particularly in younger elite sports people.
- Implicated sports include cricket, tennis, wrestling, weight-lifting, water polo, gymnastics, baseball, and wood chopping
2. Secondary Causes:
- Iatrogenic: PICC lines, transvenous pacemakers, post-mastectomy, radiotherapy.
- IV drug use
- Thoracic Inlet Anomalies: Cervical ribs, congenital fibromuscular bands, anomalous subclavius or anterior scalene muscles
- Prothrombotic States: Malignancy, hematological disorders.
- Venous stenosis from previous scarring.
Complications
- Pulmonary embolism (up to 30%).
- Chronic recurrent pulmonary embolism → pulmonary hypertension and right sided heart failure.
- Chronic venous insufficiency (swelling, pain, SVC syndrome).
Clinical Features
History
- Recent trauma or strenuous arm use
- History of thromboembolism
- OCP use in women
- Symptoms of PE (chest pain, SOB)
- Venous cannulation history
Examination
- Non-pitting upper limb edema
- Cyanosis
- Collateral vein dilation (Urschel’s sign)
- Raised hand test – persistent venous distension
- Signs of SVC obstruction (if extensive)
- Gradual symptom resolution over months (collateral formation)
- Normal arterial exam
Differential Diagnoses
- Lymphedema
- Trauma
Investigations
- Bloods: FBE, U&Es, glucose, coags, D-dimer (to exclude thrombosis as aetiology)
- CXR: Look for malignancy, cervical ribs, other obstructive lesions
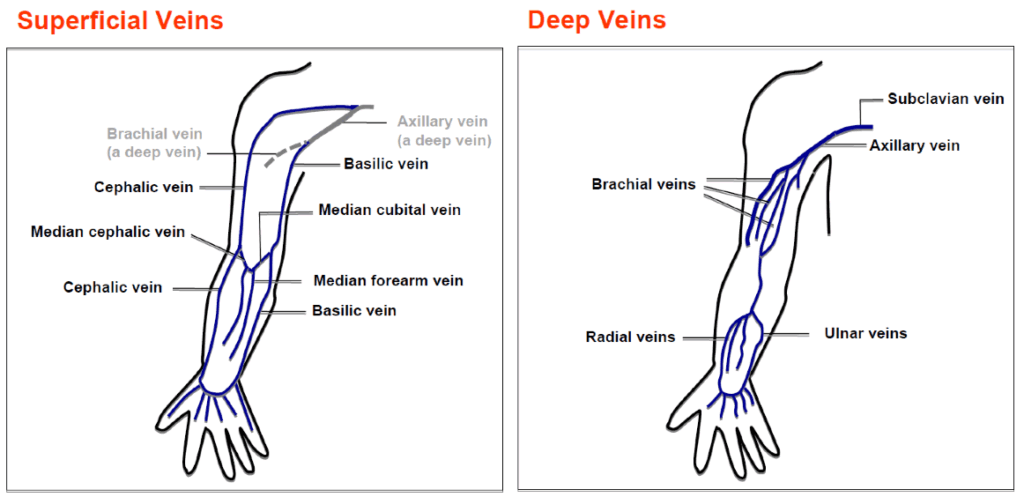
- Ultrasound: Color Doppler for initial assessment
- CT Chest/Venography: Confirm diagnosis, assess thoracic inlet, rule out PE
- MRI/MRA: Alternative if contrast contraindicated
Management
General Principles
Aggressive early intervention can restore venous patency, especially if thrombolysis is performed within 2 weeks of symptom onset. Late decompression may still benefit select cases.
Treatment Options
An aggressive approach that includes a combination of thrombolysis and thoracic outlet decompression with or without venoplasty (percutaneous, open) appears to improve long-term outcomes in patients with primary upper extremity deep vein thrombosis, particularly those with acute, moderate-to-severe symptoms
1. Anticoagulation
- All patients: therapeutic clexane + warfarin (or DOAC under haematology supervision)
- Duration: At least 3 months
2. Thrombolysis
- Consider for effort thrombosis < 2 weeks with extensive disease
- Not useful in chronic thrombosis
- Initiate IV heparin pending vascular review
3. Surgery
- Indications: Contraindication to thrombolysis, recurrent thrombosis, recurrent PE, anatomical causes
- Procedures: Embolectomy, angioplasty, stenting, rib/fibromuscular band resection
Disposition
Consult:
- Haematology
- Vascular Surgery
- Radiology (for thrombolysis)
Follow-up and ongoing monitoring as clinically indicated.

References
Publications
- Callum K, Bradbury A. ABC of arterial and venous disease: Acute limb ischaemia. BMJ. 2000 Mar 18;320(7237):764-7.
FOAMed
- Rippey J. Ultrasound Case 081. LITFL
- Rippey J. Ultrasound Case 085. LITFL
- Cadogan M. Paget-Schroetter Syndrome. LITFL
- Cadogan M. Leopold Von Schrötter. LITFL
Fellowship Notes
Educator, magister, munus exemplar, dicata in agro subitis medicina et discrimine cura | FFS |

