Casenote Bedside Ultrasound
UCEM researchers revolutionise waiting room medicine with new study
Following recent industry headlines and continual expansion of the use of bedside ultrasound in emergency medicine, UCEM researchers have risen to the challenge of the impending 4h targets (‘No, it’s not the Four Hour Rule’ or NINTFHR) to develop a validated clinical decision-making tool to improve access to impatient specialists and their thick mattress beds.
Recognising that recent years have seen Emergency staff proving that no body part is beyond assessment with a mobile scanner and that this increased workload had the potential to de-skill and unemploy our superspecialist colleagues, researchers first ‘focused their crystals’ on previously unassessed body parts with the aim of finding one that might be useful for disposition decisions.Initial trials with ‘Patient Hair Analysis – Qualitative, Objective or Facile Folly?’ (the PHAQ-OFF trial), although with initially promising results, did not yield a suitably discriminative outcome for widespread use and remains a research tool only.

Researchers then turned their attention to previously unappreciated clinical variables with impressive results.
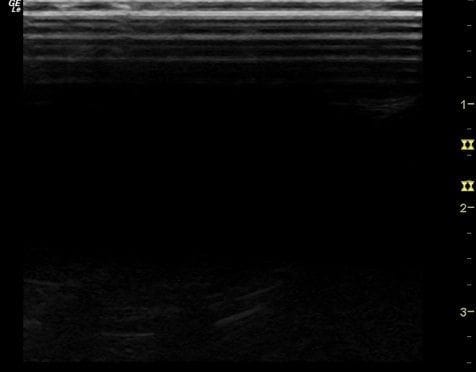
Casenote Bedside Ultrasound (the CBU score)
Portable sonography of patient’s medical records with depth analysis proved to be a high-yield discriminator and predictor for general medical admission. Using a simple, reproducible single measure (thickness >1.3cm), the need for admission for >24h after exhaustive traditional clinical assessment was found to be over 90%, compared with >2 medical staff (including NESB), this subgroup also had high enough rates of admission to merit direct referral for full workup as an inpatient.
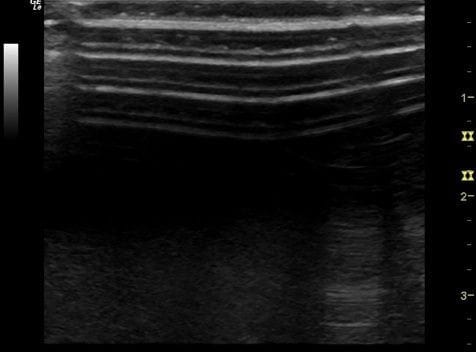
Early resistance to this as a tool in the validation study from inpatient registrars was found to be mitigated by use of the triage notes and a more formal sounding title (e.g. ‘this patient presented with SOB and has a CBU score of 4.3 so requires admission’). Improved access to medical assessment unit beds in the study hospital allowed for rapid transfer immediately after the referral to the MAU, and this 100% admission rate from the ED proved this tool’s worth as a decision making aid.
Future research is planned to assess whether this can be used either directly from triage or as a prehospital direct admission tool, aided by patients wearing bracelets with their note dimensions clearly engraved so that ambulance officers can rapidly assess the severity of their illness.
Roving reporter: Dr Duncan Campbell
UCEM Core Content
- Utopian College of Emergency for Medicine (UCEM)
- UCEM Publications and Position Statements
- UCEM Mission Statement and Essential Roles and Core Competencies
- About the Utopian College. Including Education; Examinations; and Collegial Hierarchy
- Utopian Medicine General News