CICM SAQ 2010.1 Q17
Questions
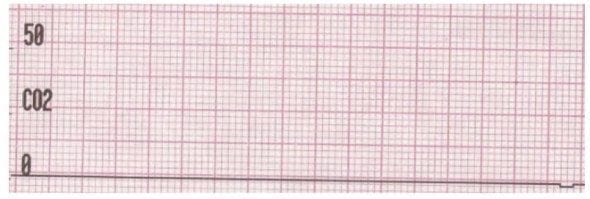
17.1. Outline four (4) causes for the capnograph trace (shown below) obtained from a critically ill patient.
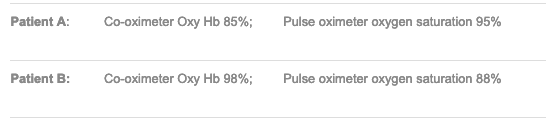
17.2. Examine the data provided from a co-oximeter and a simultaneous pulse oximeter recording from patient A and B. List three (3) causes in each patient for the discrepancy between the two oximeters.
17.3. The figure below illustrates an airway pressure waveform of a single breath during volume controlled ventilation, incorporating an end inspiratory pause and an auto- PEEP manoeuvre.
X Axis – Time in seconds
Y axis – Airway pressure in cm water
- (a) What are the factors which determine variable B?
- (b) If the delivered tidal volume was 500 ml, what is the calculated compliance?
- (c) List the change(s) you would make to the ventilator settings to treat an increase in the value of variable D.
Answers
Answer and interpretation
Outline four (4) causes for the capnograph trace (shown below) obtained from a critically ill patient.
- a) Ventilator disconnection
- b) Esophageal intubation
- c) Cardiac/respiratory arrest
- d) Apnoea test in a brain dead patient
- e) Capnograph obstruction
17.2. Patients A and B
Patient A
- CoHb
- Met Hb
- Radiofrequency interference
Patient B
- Tricuspid regurgitation
- Ambient light
- Poor peripheral perfusion
- Dyes- Methylene blue
- Poor probe contact
17.3. (a) What are the factors which determine variable B?
- Resistance, compliance, tidal volume, PEEP, insp flow rate and flow pattern
17.3. (b) If the delivered tidal volume was 500 ml, what is the calculated compliance?
- 25 ml/cm water [TV/(Plateau-PEEP)]
17.3. (c) List the change(s) you would make to the ventilator settings to treat an increase in the value of variable D.
- Increase expiratory time
- Decrease I:E ratio, decrease RR, reducing MV

Examination Library
CICM
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC