CICM SAQ 2011.1 Q8
Questions
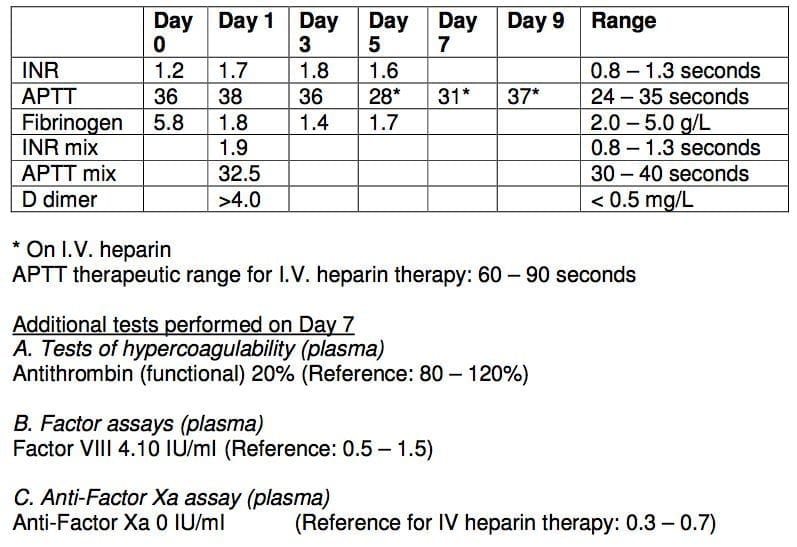
8.1. A 40 year old previously well male presents with a ruptured appendix and associated peritonitis (Day 0). He returns to theatre 3 days later with ischaemic colitis and requires a right hemicolectomy. At laparotomy, he is noted to have extensive thrombosis in his superior mesenteric vein and portal vein. Attempts to anticoagulate him postoperatively (day 5 onwards) with intravenous heparin have been unsuccessful.
His post op haematology results are as follows:
a) What are the possible factors preventing therapeutic anticoagulation in this patient?
b) List 2 strategies to effect anticoagulation with intravenous heparin.
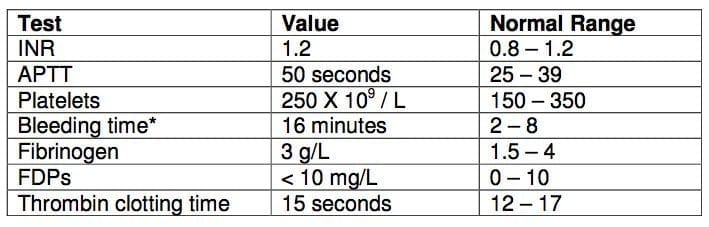
8.2. A 28 year old man presented with a persistent epistaxis to the emergency department.
The coagulation profile was as follows:
a) What is the most likely diagnosis?
b) What would you confirm your diagnosis
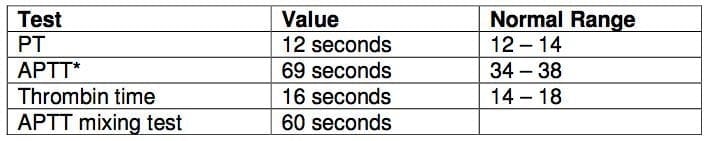
8.3. A 50 year old female presents with a right deep vein thrombosis and haemoptysis.
These blood results are from her admission:
a) What is the APTT mixing test and what is its significance in this patient?
Answers
Answer and interpretation
8.1. a) What are the possible factors preventing therapeutic anticoagulation in this patient?
- Disseminated intravascular coagulation
- High clot burden
- Antithrombin III deficiency
- High Factor VIII levels
8.1 b) List 2 strategies to effect anticoagulation with intravenous heparin.
- Change to low molecular heparin, instead of unfractionated heparin
- Give cryoprecipitate and/or fresh frozen plasma (if there is confirmed ATIII
- deficiency )
- Give antithrombin III concentrate
8.2.a) What is the most likely diagnosis?
- Von Willebrand’s disease
8.2. b) What would you confirm your diagnosis
- History – easy bruising, mucosal bleeding
- Family history
- Plasma vWF levels
- Factor VIII levels /activity
8.3. a) What is the APTT mixing test and what is its significance in this patient?
- It involves mixing patient’s plasma with normal pooled platelet free plasma. If it normalized then the elevated APTT is due to factor deficiency. Partial correction suggests an inhibitor.
- These results suggest antiphospholipid syndrome in this patient

Examination Library
CICM
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC