CICM SAQ 2013.2 Q13
Questions
13.1 A 52-year-old female was admitted the previous night with an altered level of consciousness that improved rapidly with administration of glucose.
She is referred to ICU the next day with confusion, ataxia and a worsening level of consciousness. Her CT head is normal.
The blood sugar level in the morning is 8 mmol/L on a 5% Dextrose infusion at 80 mL/hr. Her full blood count from the previous night is available as follows:
- a) List two likely causes of the coagulation abnormalities.
- b) State how you would correct the coagulopathy and give your reasoning.
—
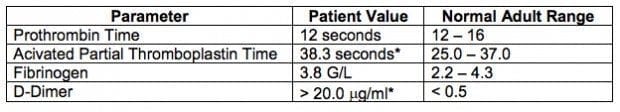
13.2 A 44-year-old male presents with dyspnoea and is diagnosed as having multiple pulmonary emboli on a computerised tomography pulmonary angiogram (CTPA). He is commenced on 1000 units of heparin per hour IVI after a 5000 unit intravenous bolus. During the night his heparin infusion has steadily increased to 1500 units per hour.
These blood results are from the following morning:
- a) Give two reasons for the relatively low APTT despite heparin therapy.
- b) List four causes for an increased predisposition to venous thromboembolic disease.
—
13.3 A 52-year-old female was admitted the previous night with an altered level of consciousness that improved rapidly with administration of glucose.
She is referred to ICU the next day with confusion, ataxia and a worsening level of consciousness. Her CT head is normal.
The blood sugar level in the morning is 8 mmol/L on a 5% Dextrose infusion at 80 mL/hr. Her full blood count from the previous night is available as follows:

- a) What is the likely cause of her confusional state?
- b) What specific treatment would you prescribe for this?
Answers
Answer and interpretation
13.1
a) List two likely causes of the coagulation abnormalities.
- Haemodilution with inadequate replacement of blood and clotting factors
- DIC
b) State how you would correct the coagulopathy and give your reasoning.
- Ensure patient is normothermic amd correct acidosis
- Platelets to increase platelet count
- FFP to replace factors II, V, VII, IX, X, and XI.
- Cryoprecipitate to replace factor VIII, and fibrinogen if FFP does not reverse INR.
- Consider tranexamic acid and/or Activated Factor 7
- Exclude on-going surgical haemorrhage
13.2
a) Give two reasons for the relatively low APTT despite heparin therapy.
- ATIII deficiency
- Increased heparin clearance
- Increased heparin binding proteins
- Technical problems such as drug preparation error, disconnected IV line, pump problem, extravasated IV cannula
b) List four causes for an increased predisposition to venous thromboembolic disease.
- Protein C def
- Protein S def
- AT III def
- Malignancy
- Factor V Leiden Lupus anticoagulant
- Immobility
- Smoking
- Cardiac failure
- Local venous obstruction
- Surgery
- Trauma
- Obesity
13.3
a) What is the likely cause of her confusional state?
- Wernicke encephalopathy.
b) What specific treatment would you prescribe for this?
- Thiamine 100 mg IV daily.

Examination Library
CICM
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC