CICM SAQ 2015.2 Q23
Question
A 70-year-old male presents to the ED with a 2-week history of increasing dyspnoea, cough with altered sputum and fever. Past history includes chronic obstructive airways disease (COPD), lung cancer seven years ago treated with chemotherapy and radiation therapy with no sign of recurrence since.
Examination findings included RR 30 breaths/min, BP 110/70mmHg, HR 145 bpm, Temp 37.4oC, anxious and distress but tired and peripherally cold and cyanosed.CXR shows findings consistent with COPD and right lower lobe infiltrate.
CXR shows findings consistent with COPD and right lower lobe infiltrate.
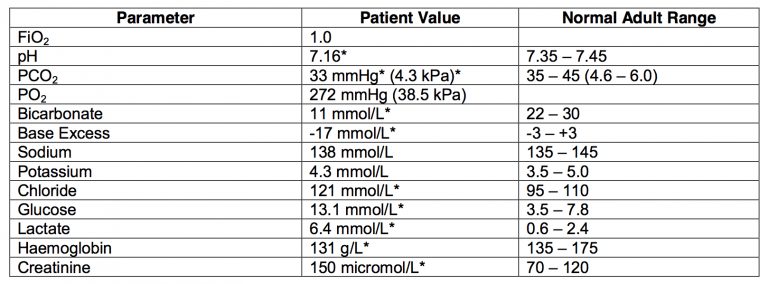
The following arterial blood gas is taken one hour after receiving 2 litres of fluid resuscitation, antibiotics and bi-level non-invasive ventilation (NIV), at FiO2 = 1.0:
- a) Give your interpretation of the arterial blood gas and outline potential causes. (40% marks)
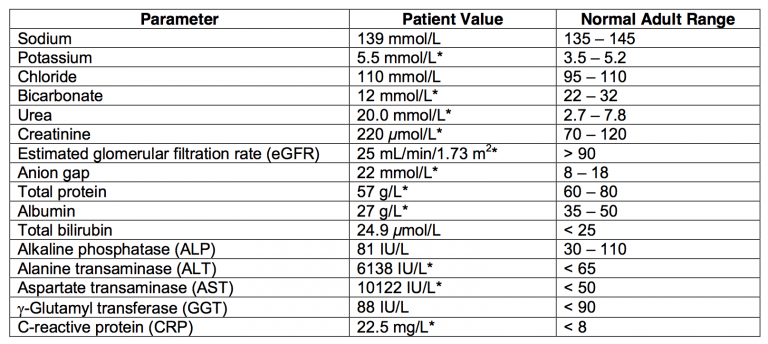
Six hours later the patient remains on NIV, is conscious, reports feeling slightly better, feet remain cyanosed, BP 105/72 mmHg, HR 108 bpm, RR 30 breaths/min, urine output 10 – 20 mL/hr and the following biochemistry profile is obtained:
- b) Give your interpretation of these findings. Include likely aetiologies. (40% marks)
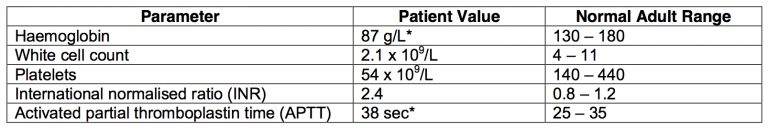
The patient’s haematology results are as follows:
- c) What is your interpretation of these findings? (20% marks)
Answer and interpretation
a) Give your interpretation of the arterial blood gas and outline potential causes. (40% marks)
ABG:
- Metabolic acidosis, normal anion gap however mixed cause (hyperchloremic predominant), high lactate and renal impairment.
- Respiratory compensation but less than expected (superimposed respiratory acidosis).
- Impaired oxygenation with moderate shunt PaO2:FiO2 272 – A-a DO2 400.
- Hyperglycemia (stress response).
Dx.
- Type 1 respiratory impairment secondary to pneumonia on background of COAD.
- Inadequate respiratory compensation due to fatigue and reduced respiratory reserve (COAD). Metabolic acidosis due to:
- Chloride excess – fluid resuscitation
- Lactate elevation – sepsis plus inadequate cardiac output.
- Renal impairment
b) Give your interpretation of these findings. Include likely aetiologies. (40% marks)
Increasing anion gap due to worsening renal impairment and possibly increasing lactate.
LFTs deranged with predominant finding of transaminitis. (This is likely to be associated with an increase in lactate).Aetiologies
Aetiologies
- Liver ischaemia due to hypoperfusion
- cardiac failure (poor output +/- liver congestion)
- severe sepsis with profound hypotension
- other shock states e.g. obstructive
- thrombo-embolic disease
Drug related e.g. paracetamol (inadvertent or deliberate)
(NB Acute alcoholic hepatitis is unlikely with such a high AST)
c) What is your interpretation of these findings? (20% marks)
Acute anaemia, acute or chronic leucopaenia, acute or chronic thrombocytopaenia, coagulopathy with raised INR
- No unifying diagnosis
- Acute drop in haemoglobin over 2 hours is most likely due to haemorrhage or massive fluid infusion.
- Massive haemolysis is less likely given the bilirubin is not raised
- Sepsis most likely cause of leucopaenia, thrombocytopaenia and raised INR
- Acute liver failure may explain raised INR
- Bone marrow failure would explain leucopaenia and thrombocytopaenia if they are chronic. Any cause of bone marrow failure also accepted.
- Pass rate: 50%
- Highest mark: 7.5

Examination Library
CICM
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC