CICM SAQ 2015.2 Q30
Question
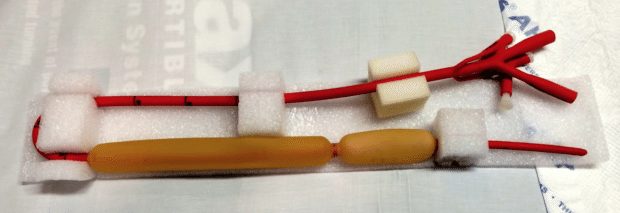
- a) What is the tube in the image above used for? (10% marks)
- b) Describe the steps for insertion of this tube. (40% marks)
- c) What are the contraindications for its insertion? (20% marks)
- d) What are the complications of its use? (30% marks)
Answer
Answer and interpretation
a) What is the tube in the image above used for? (10% marks)
Minnesota tube (Sengstaken-Blakemore or gastro-oesophageal balloon tamponade device acceptable) for balloon tamponade of bleeding oesophageal varices.
b) Describe the steps for insertion of this tube. (40% marks)
- Intubate patient to protect airway and simplify insertion.
- Check balloon for leaks & lubricate tube.
- Pass via nares (or mouth if severe coagulopathy present) and guide under laryngoscopic control
into oesophagus, until 50cm inserted. - Slowly inflate gastric balloon: 250ml air.
- Gently withdraw tube until resistance felt (~30-35cm) as balloon engages with gastro-oesophageal
junction. - Aspirate both ports. Check volume of fresh blood: reducing?
- If bleeding has ceased (~80%) then leave oesophageal balloon deflated.
- Apply traction to tubing (as below)
- If bleeding from mouth or oesophageal aspiration port continues, then inflate oesophageal balloon
with air to 25-30mmHg (max 40). - Deflate oesophageal balloon for 10 min every 2-hrs.
- Apply traction to tubing by tying 500ml bag of fluid over pulley.
- Check position on CXR: identify gastric balloon below diaphragm & radio-opaque marker along
course.
Or any acceptable technique
c) What are the contraindications for its insertion? (20% marks)
- Oesophageal stricture
- Recent oesophageal surgery
- Hiatus hernia
- Unknown cause of GI bleed
d) What are the complications of its use? (30% marks)
- Trauma to nose, pharynx, oesophagus
- Incorrect placement or dislodgement of gastric balloon in pharynx or oesophagus (may result in
acute upper airway obstruction if airway not secured) - Oesophageal tear or rupture
- Failure to control bleeding.
- Aspiration pneumonitis.
- Secondary infection: pneumonia, sinus
- Nasal or oral mucosal ulceration & necrosis from traction.
- Pass rate: 79%
- Highest mark: 9.3

Examination Library
CICM
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC