CICM SAQ 2015.2 Q4
Question
A 42-year-old male is admitted to your intensive care day 4 post induction chemotherapy for acute promyelocytic leukemia (AML-M3). The patient was initially treated with idarubicin and all-trans retinoic acid (ATRA). He has progressively become more dyspnoeic in the ward. A chest X-Ray demonstrates a bilateral, diffuse pulmonary infiltrate.Initial examination reveals:
- RR 40 breaths/min
- SpO2 88% on 10 L/min O2 by face mask
- Glasgow Coma Scale 14 (E4 M6 V4)
- Temperature 38.9 oC
- Heart rate 144 beats/min
- Blood pressure 95/50 mmHg
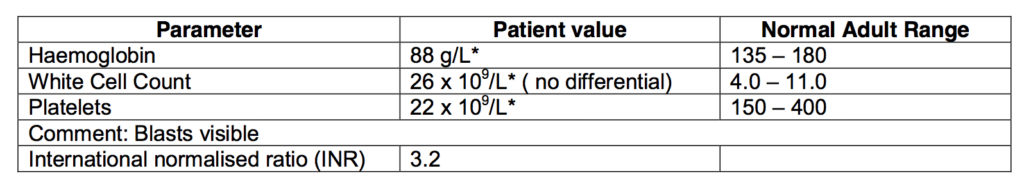
Full blood count is as follows on admission:
- Give your differential diagnosis for his respiratory failure. (40% marks)
- What are the major issues in this patient and how would you manage them? (60% marks)
Answer
Answer and interpretation
a) Give your differential diagnosis for his respiratory failure. (40% marks)
Sepsis in a patient with immune compromise secondary to leukaemia.
Nosocomial pneumonia
- Bacterial –Gm negative –E.coli, Pseudomonas, Klebsiella
- Gm positive: Strep, Staph epi
- Fungal: Aspergillus, Candida, Cryptococcus
- Atypical: Legionella, mycoplasma
- Viral: CMV, HSV, RSV, Influenza, H1N1, VZV
- PCP
- Toxoplasmosis
- TB (depending on background)
Non- infective
- Idiopathic pneumonia syndrome
- Cardiac failure (cardiotoxicity due to induction chemo)
- Diffuse alveolar haemorrhage
- Non cardiogenic capillary leak syndrome
- Chemo induced ALI / pneumonitis
- Retinoic Acid Syndrome
b) What are the major issues in this patient and how would you manage them? (60% marks)
Major issues are:
1. Hypoxic respiratory failure
- Probable nosocomial pneumonia now requiring respiratory support and is likely to be progressive
- Problem with invasive respiratory support carrying very high mortality and complications including barotrauma, further nosocomial infections
- Management – Non-invasive respiratory support commencing with CPAP progressing to BiPAP using the lowest FiO2 to maintain PaO2 above 60 mmHg. Attempt to avoid invasive respiratory support if possible.
2. Possible Sepsis
- May rapidly progress to septic shock in this patient
- Possible unusual infective agent
- Early commencement of Broad cover (Cefepime / Ceftazadime / Tazocin and Vancomycin + Voriconazole / caspofungin / liposomal amphotericin + acyclovir + Bactrim.) Discussion with ID and haematology specialists for prior antimicrobial therapy, CMV status, previous aspergillus infection etc
- Removal of indwelling intravenous catheters that are in anyway suspicious for infection
- Central access (with platelet cover), consideration of inotropes after transfusion of blood products and IV fluids preferentially using Albumin containing solutions.
- Steroids.
3. Prognosis from acute promyelocytic leukemia (AML-M3).
- Management is to liaise early with treating haematologist to ascertain likely outcome from primary disease and also discuss with family and patient the significant risk of deterioration and mortality.
4. Other
- Treatment of coagulopathy- Vit K, Platelets, FFP Difficulties in making definitive diagnosis
- Possible atypical infection with low yield probable from cultures
- Significant other non-infective differential diagnosis.
- Management includes having a high degree of suspicion for resistant or unusual organism and managing with broad cover.
- Pass rate: 37%
- Highest mark: 8.3
Additional Examiners’ Comments:
- Candidates were expected to give some indication of treatment strategies e.g. antibiotics, reversal of coagulopathy rather than just writing D/W ID, haematology etc.
Examination Library
CICM
Chris is an Intensivist and ECMO specialist at the Alfred ICU in Melbourne. He is also a Clinical Adjunct Associate Professor at Monash University. He is a co-founder of the Australia and New Zealand Clinician Educator Network (ANZCEN) and is the Lead for the ANZCEN Clinician Educator Incubator programme. He is on the Board of Directors for the Intensive Care Foundation and is a First Part Examiner for the College of Intensive Care Medicine. He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives.
After finishing his medical degree at the University of Auckland, he continued post-graduate training in New Zealand as well as Australia’s Northern Territory, Perth and Melbourne. He has completed fellowship training in both intensive care medicine and emergency medicine, as well as post-graduate training in biochemistry, clinical toxicology, clinical epidemiology, and health professional education.
He is actively involved in in using translational simulation to improve patient care and the design of processes and systems at Alfred Health. He coordinates the Alfred ICU’s education and simulation programmes and runs the unit’s education website, INTENSIVE. He created the ‘Critically Ill Airway’ course and teaches on numerous courses around the world. He is one of the founders of the FOAM movement (Free Open-Access Medical education) and is co-creator of litfl.com, the RAGE podcast, the Resuscitology course, and the SMACC conference.
His one great achievement is being the father of three amazing children.
On Twitter, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC