Contrast Agents
OVERVIEW
Contrast agents are substances used in medical imaging as to enhance the contrast or the distinction between different tissues.
- aka contrast medium
RADIOGRAPHIC CONTRAST AGENTS
Composition
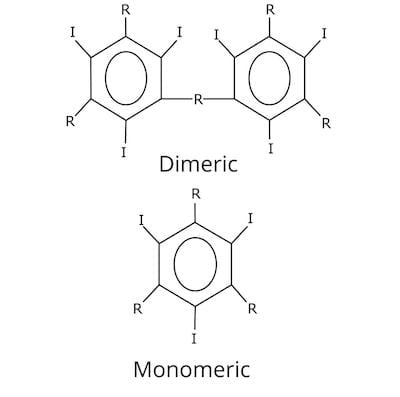
- Currently available agents contain a tri-iodinated benzene ring (either monomeric or dimeric; ionic or non-ionic)
- Ionic agents disperse into negative and positive ions — and have a higher toxicity — the non-ionic agents do not
- Additional components of contrast media allow large volumes of contrast to be administered quickly and with minimal toxicity
- Low osmolar contrast agents are typically used as they decrease osmolality, which is associated with adverse reactions
Use
- Iodine-based contrast agents are typically used for CT contrast scans and for urological studies such as IV pyelograms
- The allow for angiography and the demarcation of tumours
- Volume injected typically ranges from 50 ml to 150 ml, depending on the type of scan
- Oral contrast agents are also used to delineate gastrointestinal structures as they coat the luminal walls of the intestines
Adverse reactions to the injection of iodine-based contrast agents
- they include
- nausea, vomiting
- pruritis
- vasovagal episodes
- laryngeal edema
- anaphylactic shock
- nephrotoxicity (see Contrast-induced nephrotoxicity)
- extravasation injury
- most occur <15 min after administration of the agent
- frequency
- occur in ~ 5% of patients
- 0.05% are severe
- mortality rate is 1/75,000 injections
- high-risk patients include:
- history of a severe-adverse contrast reaction
- active asthma
- multiple drug or environmental allergies
- risk of an adverse reaction to a repeat administration of intravenous contrast agent is ~ 15% (i.e. 3 x baseline risk)
- premedication with steroids is recommended in patients with prior adverse reactions if the study is absolutely necessary
- e.g. 50 mg prednisone PO, 12 and 2 hours before the procedure
GADOLINIUM-BASED CONTRAST AGENTS
These agents used to have the same effect as radiographic contrast agents, but for MRI
- Gadolinium is a toxic, rare earth metal that is safe to administer intravenously when attached to a chelate
Use
- Gadolinium chelates are used in nearly examinations of the brain and soft tissues
- no usually needed for imaging the bones and joints
- lower volumes required compared to riodine-based agents, usually <15 mL (dose is based on weight)
- oral contrast agents are not usually administered, although Barium and milk can be used
Adverse effects
- Minimal risk in patients with norma renal function
- occasional episodes of vomiting and hives reported
- anaphylaxis is very rare
- Nephrogenic systemic fibrosis
- may affect patients with renal failure (serum Cr >3.0 mg/dl and GFR <30 ml/min)
- >200 cases described, all associated with IV administration of a gadolinium chelate within 2 or 3 months before onset of symptoms
- features include skin thickening, joint contracture, and severe pain
- risk increases with repeat exposure
- gadolinium chelates should be avoided in patients with moderate to severe renal failure
CONTRAST MEDIA EXTRAVASATION
Potential complication of CT contrast scans
- occurs in about 1 in 200 CT contrast scans
- rare with MRI, due to the low volume of contrast injected
- due to automated power injection, large volumes can extravasate in a short period of time
- risk factors
- patient factors: elderly, emaciated, oedematous, confused
- site of venous access: back of the hand, wrist, foot and ankle (more fragile veins with less subcutaneous tissue)
- gauge of IV catheter: higher with small gauge cannula (22G or smaller)
- high-osmolar contrast medium (less risk if pre-warmed to reduce viscosity)
- pre-warming of high-osmolar (370 mg/ml) lowers the viscosity and has been proven to lower the probability of extravasation
Management (according to local protocol)
- stop contrast infusion and notify the radiologist immediately
- complete the acquisition of images
- apply an ice pack to the affected area
- elevate the affected extremity to reduce swelling (attempted aspiration of the extravasated media is not effective)
- observe the patient for at least 2h
- consider plastic surgery consultation if extravasations involves >100 ml of contrast agent
- notify the treating doctor requesting the study
- follow up the patient in the next few days until the resolution of local oedema
- patients should seek medical attention if:
- increasing swelling or pain over time
- blistering, ulceration, induration or other skin changes
- altered tissue perfusion and/or changes in sensation
References and links
LITFL
Journal articles
- Boehm, I (2008). Seafood Allergy and Radiocontrast Media: Are Physicians Propagating a Myth? The American Journal of Medicine. 121 (8): e19. doi:10.1016/j.amjmed.2008.03.035. PMID: 18691465
- Brockow, K.; et al. (2005). Management of hypersensitivity reactions to iodinated contrast media. Allergy. European Journal of Allergy & Clinical Immunology. 60 (2): 150–158. doi:10.1111/j.1398-9995.2005.00745.x. PMID: 15647034
- Morcos SK, et al, and members of the Contrast Media Safety Committee of the European Society of Urogenital Radiology (ESUR). Dialysis and Contrast Media. Eur Radiol 2002;12(12):3026-30. PMID: 12439587
- Thomson, K; Varma, D (2010). “Safe use of radiographic contrast media”. Australian Prescriber, 33:19-22. Available at http://www.australianprescriber.com/magazine/33/1/19/22/
- Younathan CM, et al. Dialysis is not indicated immediately after administration of nonionic contrast agents in patients with end-stage renal disease treated by maintenance dialysis. AJR Am J Roentgenol 1994;163(4):969-71. PMID: 8092045
FOAM and web resources
- Renal Failure Network — Prophylactic hemodialysis for iv contrast exposure? (2009)

Critical Care
Compendium
Chris is an Intensivist and ECMO specialist at The Alfred ICU, where he is Deputy Director (Education). He is a Clinical Adjunct Associate Professor at Monash University, the Lead for the Clinician Educator Incubator programme, and a CICM First Part Examiner.
He is an internationally recognised Clinician Educator with a passion for helping clinicians learn and for improving the clinical performance of individuals and collectives. He was one of the founders of the FOAM movement (Free Open-Access Medical education) has been recognised for his contributions to education with awards from ANZICS, ANZAHPE, and ACEM.
His one great achievement is being the father of three amazing children.
On Bluesky, he is @precordialthump.bsky.social and on the site that Elon has screwed up, he is @precordialthump.
| INTENSIVE | RAGE | Resuscitology | SMACC
